热门问题
时间线
聊天
视角
精神分裂症
一种精神疾病 来自维基百科,自由的百科全书
Remove ads
精神分裂症(schizophrenia,台湾称思觉失调症)是一种常见的重性精神障碍[11][12],属精神病性障碍大类[13]。其典型症状为精神病性症状(psychosis)[1],即无法区分真实与虚幻[14],且伴有多种精神状态的紊乱,涉及思维(如妄想、思维形式紊乱)、感知(如幻觉)、自我体验(如感觉、冲动、思想或行为受外力控制的体验)、认知(如注意力、语言记忆和社会认知受损)、意志力(如动机丧失)、情感(如情绪表达迟钝)和行为(如怪异或无目的的行为、不可预测或不适当的干扰行为组织的情绪反应)[15]。精神分裂症常与其他精神障碍共病,例如焦虑障碍、重性抑郁障碍或物质使用障碍等[16]。症状通常逐渐地出现,且一般在成年早期开始,并持续一段长时间[2][5]。
精神分裂症的成因包括环境因子及遗传因子[3]。可能的环境因子包括在城市中长大、滥用娱乐性药物、某些传染病、父母年龄,和自身在母体内时营养摄取不足[3][17]。遗传因子则包括各种常见和罕见的遗传变异[18]。精神分裂症可依据求诊者所表现出来的行为及其所主诉的个人经历作诊断[5]。在诊断时,还必须把求诊者的文化背景纳入考虑范围之内[5]。截至2013年为止,此病并没有任何客观的测试予供作诊断[5]。精神分裂症完全不同于分离性身份障碍(旧称“多重人格障碍”,俗称“人格分裂”)——这种混淆的想法常在公众的认知中出现[19]。
治疗的重心是为患者处方抗精神病药,以及安排咨询、工作培训和社会康复[1][3]。目前尚不清楚典型抗精神病药与非典型抗精神病药两者间哪种的效果会较佳[20]。在其他抗精神病药物都无法改善病情的情况下,就可能会使用氯氮平。必要时,可能会强制患者住院治疗,如患者可能会对自身或他人构成伤害这一种情况,但现在的住院时间比以往更为短暂,且强制住院治疗的总次数亦较为少[21]。
世界人口中约0.3~0.7%在其一生中受精神分裂症所影响[9] 。2019年,全球估计有2000万名精神分裂症患者[22]。男性比女性更常受到精神分裂症的影响[1],且其病情也一般较严重。大约20%的人康复得很好,一些人亦能完全康复[5];50%的人则终生受到一定程度的影响[23]。患者常伴有一定的社会问题,例如长期失业、贫穷和无家可归[5][24]。患有精神分裂症的人的平均预期寿命比平均值少10年至25年[8]。其背后原因是患者的身体健康问题增加和自杀率较高(约5%)[9][25]。在2015年,全球估计有17,000人死于与精神分裂症有关或由其引起的行为[10]。
Remove ads
名称
1896年,德国精神病学家Kraepelin因该障碍多起病于青少年且以衰退为结局,将其命名为“早发性痴呆”[11][12]。1911年,瑞士学者Bleuler研究认为核心问题是人格与思考、记忆、感知的分裂,[26]提出了“精神分裂”(splitting of mind)的概念,又因预后并不一定是衰退,故建议命名为“schizophrenia”[11]。该障碍的英文名“schizophrenia”即移植自Bleuler的新拉丁文名,词根是希腊语“skhizein”(意为“分裂”)与“phrēn”(意为“精神”)[27][26]。
中文各地过去都直译作“精神分裂症”。由于易与分离性身份障碍(“人格分裂”)混淆,且病患认为该词易受污名化等原因[28],台湾于2014年改称“思觉失调症”。[29][30][31]香港自2001年[31]使用“思觉失调”一词指代“psychosis”[32](台湾、中国大陆译“精神病”)或“早期psychosis”[33](台湾、中国大陆无专名),但仍将此障碍称作“精神分裂症”。
Remove ads
症状

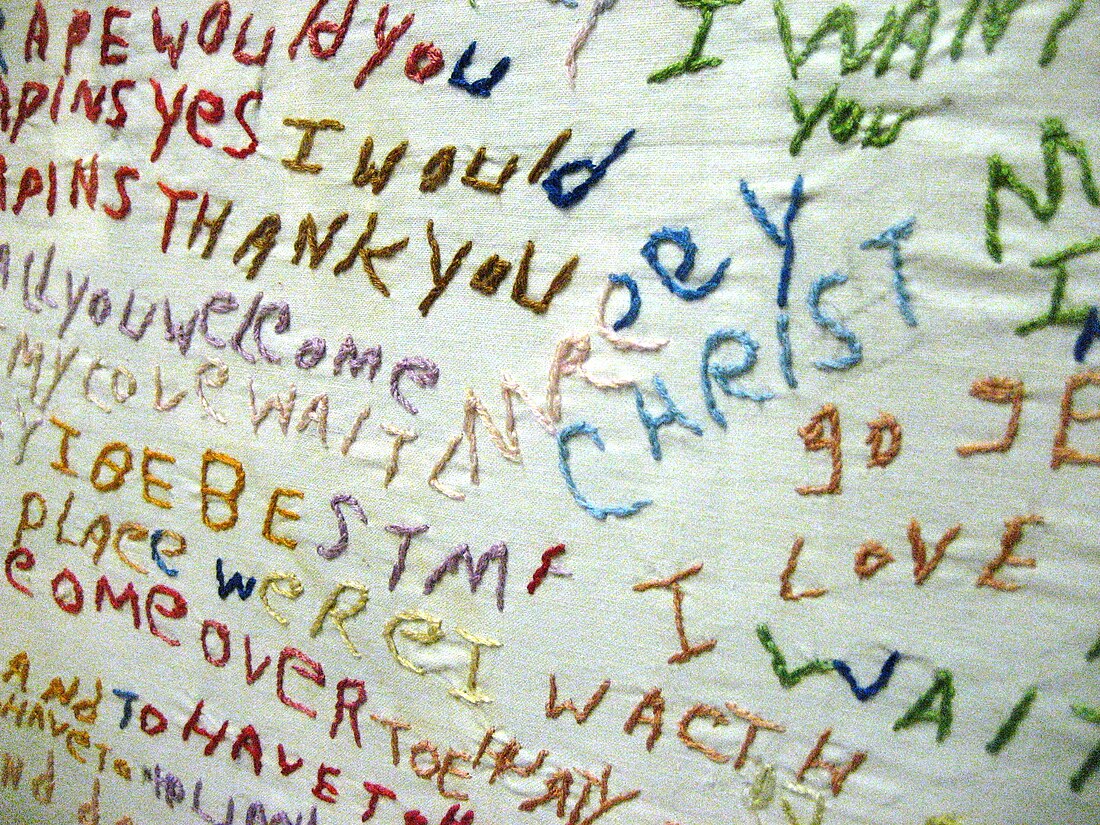
精神分裂症患者可能会出现的症状包括幻觉(以幻听最为多见)、妄想(以被害妄想与关系妄想最为多见),以及思维和言语紊乱。思维和言语紊乱的程度可从较轻微的思维不清晰,以至较严重的胡言乱语。患者亦普遍出现社交退缩、对穿衣和卫生不感兴趣,以及失去动力和判断力的情况[34][35]。
精神分裂症患者亦常见出现自我体验异常的症状,例如认为一些想法或感觉不是真正属于自己的,而是他者所植入的,这种症状有时称为“被动体验”[36]。常在患者身上观察出情感障碍,例如缺乏积极的情绪反应[37]。社会认知障碍也与精神分裂症有关[38],例如患者所表现出来的多疑症状。患者亦常面临社会孤立。普遍患者还在以下范畴出现困难:工作记忆、长期记忆和学习、管控功能、注意力[9]。在一种罕见的亚型中,患者会经常保持缄默、在异常姿势中保持不动,或者表现出亳无理由的兴奋状态——都是紧张性抑鬱障碍的症状[39]。患者亦会发现自己对面部表情的感知存有一定困难[40]。部分患者会出现思想阻断的现象,亦即其在说话时会突然停顿数秒至数分[41][42]。
大约30%至50%的精神分裂症患者不能接受自己患病的事实,或遵从推荐予他们的治疗[43]。精神分裂症的治疗可能会对患者的洞察力产生一些影响[44]。
精神分裂症患者可能比一般人有较高的比率患上大肠激躁症,但除非特别提及此一问题,否则他们通常不会特别指出[45]。精神性多渴症在精神分裂症患者中相对较普遍[46]。
Remove ads
精神分裂症通常以阳性及阴性症状来描述[47]。阳性症状是大多数人通常不会遇到的症状,但存在于精神分裂症患者中。这包括妄想、思维和言语紊乱,以及在五感上存有幻觉——这些通常被认为是精神分裂的表现[48]。幻觉通常与妄想的主题内容有关[49]。药物对治疗患者的阳性症状十分有效[49]。
阴性症状是指正常情绪应答或其他思维过程中所存有的一些缺陷,药物对治疗阴性症状的效果较差[35]。其包括缺乏情感或情绪淡然(Reduced affect display)、贫语症(Alogia)、享乐不能(Anhedonia,快乐不起来)、无社会性(Asociality)和动机缺乏(Avolition)。与阳性症状相比,阴性症状对他人的负担、患者的生活品质以及工作能力的影响较大[50]。拥有较为严重的阴性症状的患者在发病之前通常具有适应不良的生活史,并且药物对其治疗效果通常亦是十分有限[35][51]。
多于一项的变量分析研究对“阳性及阴性”这一区分表示质疑,并按其观察把症状分成三个维度。尽管用语会有所差异,但大多会将其分成人格解体、幻觉及阴性症状[52]。
一般认为认知能力的缺陷是精神分裂症的核心特征[53][54][55]。患者的认知缺陷程度是个体功能、工作表现的品质,以及维持治疗效度的预测因素[56]。认知功能障碍的存在及其程度是一项比起阳性或阴性症状更为良好的指标去评估个体功能[53]。受认知功能缺陷所影响的范畴十分广泛,其中包括工作记忆、长期记忆[57][58]、口语叙述记忆[59]、语意处理过程[60]、情节记忆[56] 、注意力[23] 、学习能力(特别是语言学习)[57]。在精神分裂症患者中最明显的是言语记忆的缺陷,并且不是由注意力不足所致。言语记忆障碍与患者的语意编码能力(即处理与意义有关的信息的能力)下降有关,其被视为长期记忆缺陷的另一已知原因[57]。当给予受试者上面写有一列单词的列表时,健康的人会较常记住一些意思积极的词语(此现象称为波丽安娜效应);然而,精神分裂症患者倾向于不管其涵意如何,一概记住所有词语,这表明失去愉悦感会使患者对词语的语义编码能力受损[57]。这些缺陷在患者的病情发展至某种程度前就能发现[53][55][61]。精神分裂症患者的一级亲属和其他高危群体亦表现出一定程度的认知能力缺陷,特别是在工作记忆上[61]。关于精神分裂症患者的认知缺陷的文献综述显示,该缺陷可能在青春期早期,或早至儿童期时就已经存在[53]。即使随着时间的推移,认知缺陷在大多数患者中仍倾向保持原来的样子,少部分患者或因基于环境变数的可识别原因而改变[53][57]。
虽然“随着时间的推移,认知缺陷仍倾向保持原来的样子”的证据是可靠和充分的[56][57],但在这个领域的大部分研究都集中于提高注意力和工作记忆的方法[57][58]。研究人员曾利用“设立较高或较低的奖赏”以及“提供教育与否”等环境变数去尝试改善患者的学习能力,结果显示:较高的奖赏会使患者的表现更差,而提供教育则能改善患者的表现,这显示可能存在一些改善认知表现的治疗[57]。可通过口语表达训练,改善患者的思维、注意力和语言行为;亦可通过认知复诵(cognitive rehearsal),给予患者自我教导(self-instructions),其能使患者在处理困扰的处境时有一套应对表现,以及令在患者在成功时自我强化(self-reinforcement):这都能显著提高回忆任务(recall tasks)的表现[57]。这种类型的训练称为“自我教导训练”(self-instructional training),它所产生的好处包括能使患者毫无意义的言语减少,以及改善患者的回忆能力和注意力[57]。
Remove ads
青春期晚期至成年人早期是精神分裂症发病的高峰[9],这亦是青壮年人社会和职业发展的关键年龄[62]。经诊断患有精神分裂症的人中,分别有40%和23%的男性及女性在19岁之前就表现出该病的症状[63]。精神分裂症的症状一般在16-30岁期间首次出现[2][5]。大多男性患者在18-25岁期间发病,女性患者则大多在25-35岁之间发病[64]。为了让与精神分裂症相关的发展障碍的程度减至最低,研究人员已经进行了许多用以鉴定和治疗该病的前驱期的研究,使精神分裂症在早至发病前30个月就能发现[62]。在发病前,当事人可能会经历可以自我控制或短暂的精神分裂症状[65],和社交退缩、易怒、烦躁不安、动作笨拙这些非特异性症状[66][67]。发展精神分裂症的儿童可能会有的表现包括智力下降、动作发展迟缓、偏好于独自玩乐、社交焦虑和学习成绩差[68][69][70]。
病因
据估计,精神分裂症的遗传度为80%,这表示80%的精神分裂症个体患病风险差异可由基因方面的差异来解释[73]。该些估计的差异很大,因为难以把遗传因子和环境因子的影响区分[74]。发病的最大单一危险因子是一级亲属(包括父母、子女和手足)中有人患有精神分裂症(风险为6.5%);若同卵双胞胎中其中一方是精神分裂症患者,另一方则有超过40%的机会也受到精神分裂症的影响[19]。如果双亲中其中一位患有精神分裂症,其子女患上精神分裂症的风险约为13%;如果双亲分别都患有精神分裂症,风险则将近50%[73]。若急性短暂性精神分裂患者拥有与精神分裂症有关的家族病患史,其在一年后诊断为精神分裂症的几率约有20%-40%[75]。有关精神分裂症候选基因的研究结果一般不能找到一致的相关性[76]。
目前已知许多基因与精神分裂症有关,每组都对精神分裂症有少许的影响,以及人类现时尚末完全了解每组基因的传递和表达[18][77]。多基因遗传评分的结果显示,该些基因最少可以解释7%精神分裂症的易患性变异[78]。约5%的精神分裂症个案可部分归因于罕见的拷贝数变异,包括22q11、1q21以及16p11[79]。该些罕见的拷贝数变异会使个体发展精神分裂症的机会增加最多20倍,当事人亦常伴发孤独症和智能障碍[79]。
2018年6月,《科学》期刊发表一篇元分析初步发现,精神分裂症和双相障碍、重郁症、注意缺陷多动障碍有许多共同的可能致病基因[80]。2024年,大脑转录组学相关研究提示,要发展出精神分裂症、双相障碍和孤独症谱系障碍等精神障碍,女性比男性可能需要更多遗传因素与环境因素共同作用[81]。
Remove ads
与精神分裂症的病发相关的环境因子包括生活环境、使用药物,以及产前应激[9]。
母体应激跟患上精神分裂症的风险增加有关,而这可能是络丝蛋白所致的[82]。孕妇营养缺乏和肥胖皆可能是精神分裂症的风险因子。现有证据亦表明母体应激及感染会令像白细胞介素-8和肿瘤坏死因子般的促炎症蛋白质产生,继而影响胎儿的神经发展[83][84]。
虽然养育方式对精神分裂症的病发并没有任何重大的影响,但拥有鼓励型的父母的人,在与拥有批评型或敌对型的父母的人相比之下,他日后的病发机会更低[19]。在儿时心灵受创、父母死亡、成为欺凌或辱骂对象的人,其日后罹患精神分裂症的风险会增加[85][86]。即使考虑到像吸毒、种族和社会群体规模般的因素[87],在城市环境中渡过童年生活的人或住在城市的成年人,罹患精神分裂症的风险仍会增加至原本的两倍[19][9]。其他重要因素包括社会孤立、社会逆境相关的移民、种族歧视、家庭困难、失业,和居住条件恶劣[19][88]。
已有假设指出,在一些人当中,精神分裂症的病发与肠道功能障碍有关,例如非乳糜泻的麸质敏感或肠道菌群异常[89]。精神分裂症患者亚组对麸质的免疫应答不同于乳糜泻患者,麸质过敏症患者的某些血清生物标志物会升高,例如抗麦醇溶蛋白IgG或抗麦醇溶蛋白IgA[4]。
Remove ads
大约一半的精神分裂症患者吸毒、滥药或摄取过多的酒精[90]。安非他命、可卡因和较小程度的酒精可导致短暂的刺激性精神障碍或与酒精相关的精神障碍,其与精神分裂症十分类似[19][91]。精神分裂症患者使用尼古丁的速度比普通人群高出许多,虽然这通常不认定为病因[92]。
酒精滥用可能会通过诱发机制,引起活性物质所致的慢性精神障碍[93]。 但使用酒精与早年发病的精神障碍并不相关[94]。
大麻可能是精神分裂症的其中一个诱发因素[17][95][96]。其可能会令高危人士患上精神分裂症[96]。患病风险可能在配合某些基因的情况下才会增加[96],或可能与先前存在的精神病理有关[17]。早年接触大麻与患病风险的增加密切相关[17]。所增加的程度仍是末知[97],但患上精神障碍的风险估计是增加了2-3倍[95]。吸食较高剂量的大麻以及吸食频率较高这两项因素与患上慢性精神障碍的风险增加有关[95]。
若胎儿在母体内发育期间经受缺氧不良因素影响,则可能会增加患上精神分裂症的风险[9]。经诊断确实患上精神分裂症的人更可能在冬季或春季出生(至少在北半球情况如是),其可能是胎儿接触病毒所致[19]。患病风险因此会增加约5%-8%[99]。若怀孕期间或出生时胎儿受到像弓形体般的病原体所感染,其日后的患病机会增加[100]。
病理机制
尽管精神分裂症的病理机制尚是不明,但研究人员已经进行了许多尝试去解释大脑功能改变和精神分裂症之间的关系[9]。当中最常见的解释就是多巴胺假说,该假说把精神病中所出现的心智缺陷解释成是因多巴胺能神经元(dopaminergic neurons)异常所致[9]。其他可能的机转则涉及到神经递质谷氨酸和神经发展过程。现有框架已假设该些生理上的异常与症状是相关的[101]。
研究者依据急性精神分裂期间患者的多巴胺水平会上升,及影响多巴胺受体的药物对治疗精神分裂症是有效果的观察,来把多巴胺信号异常跟精神分裂症划上联系[102][103]。此外他们亦假设多巴胺信号异常为患者出现妄想的根本原因[104][105][106]。患者前额叶皮质的多巴胺受体D1水平下降可能为工作记忆能力减退的原因[107][108][109][110]。
现有各种证据支持NMDA受体信号会在精神分裂症患者中减退。研究表明,NMDA受体的表达减少和NMDA受体阻滞剂的运用能够模拟精神分裂症的症状及与其有关的生理异常[111][112][113]。尸检研究一致证实该些神经元的亚型除了形态异常外,亦不能表达GAD67[114]。在工作记忆任务中须进行的神经元集群同步会运用到某些中间神经元,而该些中间神经元在精神分裂症患者中出现异常[114][115][116][117]。
证据也显示神经发育异常会对精神分裂症的发病存有影响。精神分裂症患者在发病以前一般就已出现了认知障碍、社会功能障碍、运动技能障碍[118]。像母体内感染[119][120]、孕妇营养不良、怀孕期间出现并发症般的问题皆会使胎儿于日后患上精神分裂症的风险增加[83]。精神分裂症一般始发于18-25岁期间——这跟某些与精神分裂症相关的神经发展阶段重叠[121]。
精神分裂症患者常出现管控功能方面(包括计划能力、抑制能力、工作记忆能力)的缺陷。尽管该些功能为可分离的,但患者在相关方面出现障碍这点,可能反映了其工作记忆中表达目标相关信息的能力下降,且在利用它来指导认知和行为方面出现困难[122][123]。该些障碍与许多神经影像学和神经病理学上的异常有关。譬如功能性神经成像研究已发现患者的神经处理有效性减少的证据:他们的背外侧前额叶需激活至相对较高的水平,才能应付与工作记忆任务有关的控制。该些异常可能跟众验尸结果中所发现的神经毡密度减少有关——后者可通过锥状细胞密度增加和树突棘密度减少来证明。这些细胞和功能异常也可能反映在结构性神经影像学研究中,该些研究发现与工作记忆任务表现相关的灰质体积减少[124]。
研究已把阳性及阴性症状跟颞上叶及前额叶基底部的脑皮质厚度减少划上联系[125][126]。尽管文献上经常会形容精神分裂症患者是享乐不能的,然而大量证据表明精神分裂症患者的享乐应答仍然完好[127],并指享乐不能是反映了与奖励有关的其他过程存有障碍[128]。总体而言,尽管精神分裂症患者的享乐应答完好,但奖励预测机制可能存有缺陷,使其欠缺动机[129]。
Remove ads
诊断
精神分裂症是根据美国精神医学学会的精神障碍诊断与统计手册第五版(DSM-5)或世界卫生组织的国际疾病和相关健康问题统计分类(ICD-10)中的标准而作诊断。这些标准的依据为求诊者所主诉的个人经历和他人对求诊者的异常行为描述,之后由精神卫生专业人员进行临床评估。在诊断前,与精神分裂症相关的症状必须在患者中不断发生,并需达到一定的严重程度[19]。截至2013年为止,此病并没有任何客观的测试予供作诊断[5]。
2013年,美国精神医学学会发布了精神障碍诊断与统计手册第五版。必须在至少一个月的大部分时间内满足两项诊断标准,以及至少六个月对社会或职业功能有显著影响,才能诊断求诊者患有精神分裂症。若要诊断成患有精神分裂症,必须具有以下症状中的其中一项:妄想、幻觉或言语散乱。其他用以作诊断的症状包括阴性症状、紧张性行为或行为紊乱[130]。定义基本上与2000年的精神障碍诊断与统计手册(DSM-IV-TR)相同,但是第五版做出了许多改变。
- 亚型分类——如偏执型或紧张型精神分裂症等,都遭到去除。这些在以前的修订中得以保留的原因是基于惯例,但后来经事循证明,亚型在疾病的治疗上是没有价值的[131]。
- 僵直症不再与精神分裂症密切相关[132]。
- 在对精神分裂症患者的病程进行描述时,建议更好地区分病症的当前状态及其过去发展,令整体描述更为清楚[131]。
- 不再建议对施耐德主要症状(Schneider's first-rank symptoms)进行特殊治疗[131]。
- 为了更明确地把分裂情感性障碍与精神分裂症划分,故完善了分裂情感性障碍的定义[131]。
- 它向医护人员推荐了一项涵盖精神病理学八个领域的评估,用以帮助临床决策[133]。
在欧洲国家,ICD-10的诊断标准较为常用;在美国和世界各地,DSM的诊断标准则较ICD-10的常用,并广泛应用于研究中。ICD-10的诊断标准更为重视施耐德主要症状。在医学实践中,两套系统之间的一致性很高。[134]目前正在草拟中的ICD-11,提倡在关于精神分裂症的诊断标准中添加“自体障碍”(self-disorder)这一种症状[36]。
如果困扰患者的症状存在超过一个月,但少于六个月,则应诊断为类精神分裂症。若精神症状持续不到一个月,则可能诊断为短暂精神分裂,患者所拥有的各种症状则可归类为未特指的精神分裂症。如果情感性症状与分裂症状并存,则会诊断为分裂情感性障碍。如果精神上的症状是一般医学病症或物质所直接导致的,则诊断为继发性精神障碍[130]。如果求诊者出现广泛性发育障碍的症状,则不能诊断为精神分裂症,除非求诊者还明显地出现了妄想或幻觉等症状[130]。
DSM-5已删去DSM-IV中提出的所有亚型[135]。DSM-IV-TR中所包含的五个亚型如下[136][137]:
- 偏执型:又称妄想型,患者出现妄想和幻觉,但是没有出现思维障碍、行为紊乱或是情感淡漠。妄想的主题是也许是把事物夸张化,亦有可能令患者感到受迫害。(DSM代码:295.3/ICD代码:F20.0)
- 紊乱型:在ICD中称作青春型,症状既有思维障碍,亦有情感淡漠,严重时可出现无法阅读文章,观看电影电视的情况。认知能力虽然在服药后会得到改善,但与患病前不可同日而语。认知能力损害是对患者影响最大的症状。(DSM代码:295.1/ICD代码:F20.1)
- 紧张型:患者几乎僵直不动或者过于兴奋,漫无目的地行动,以及脸部表情和躯体动作异常,症状还包括紧张型木僵或蜡状屈曲(waxy flexibility)、模仿别人说话及动作等。(DSM代码:295.2/ICD代码:F20.2)
- 未分型:存在精神症状,但是不符合上面几种分类(DSM代码:295.9/ICD代码:F20.3)
- 残余型:阳性症状仅以轻度的形式存在(DSM代码:295.6/ICD代码:F20.5)
ICD-10中所包含的亚型[136]:
- 精神分裂症后抑鬱症:精神分裂症发病以后所出现的抑鬱发作,当中仍存有轻度精神分裂症的症状。(ICD代码:F20.4)
- 单纯型:阴性症状隐匿地持续发展,在此以前没有精神病发作史。(ICD代码:F20.6)
俄罗斯版的ICD-10中亦包含了呆滞型精神分裂症,而其属于ICD-10第5章F21节——“分裂型”障碍这一索引栏目中[138]。
几种不同的精神障碍的患者之中亦有可能出现跟精神分裂症患者类似的心理症状,包括边缘性人格障碍[139]、双相障碍[140]、物质诱发的精神分裂、药物中毒。妄想障碍、回避性人格障碍、类精神分裂型人格障碍、社交焦虑障碍的社会退缩等,亦会令该病的患者出现“妄想”这一种症状(非怪异妄想)。类精神分裂型人格障碍的症状与精神分裂症类似,但相对而言不太严重[5]。虽然精神分裂症患者伴发强迫症的常见程度远高于可用“巧合”来解释,但难以区分强迫症中所出现的强迫观念和精神分裂症中所出现的妄想[141]。一些人不再服用苯二氮卓类药物后,会出现可持续一段长时间的严重戒断症状。戒断症状类似于精神分裂症,故有可能因此而误诊[142]。
可能需要进行更全面的医学和神经学检查,以排除求诊者患上跟精神分裂症的临床表现差异不大的疾病,如代谢疾病、全身性感染、梅毒、人类免疫缺陷病毒感染、癫痫、边缘性脑炎、大脑损伤。中风、多发性硬化症、甲状腺功能亢进症、甲状腺机能低下症以及像阿兹海默病、亨丁顿舞蹈症、额颞痴呆、路易氏体痴呆般的痴呆的表现皆可能类以于精神分裂症[143]。可能有必要排除求诊者出现谵妄,其可通过幻视、急性发作以及知觉水平波动这些特点与精神分裂症区分,亦能把它视为求诊者患上其他潜在性疾病的迹象。除非精神分裂症患者有特殊的医学征兆或可能对抗精神病药物存有不良应答,否则通常不会复发。对处于儿童阶段的求诊者而言,专业人员必须把典型的童年幻想跟幻觉分开看待[5]。
预防
精神分裂症在社会健保层面是难以预防的,因为没有可靠的迹象可用于鉴定属于酝酿期(prodromal)的思觉敏感(at-risk mental state)阶段[144]。可以确切介入患者最早的时间是初次出现精神分裂(psychosis)症状时。psychosis不全是由于精神分裂症导致。Cochrane 2020年的综述表示,如果此时提供帮助,可以使患者在日后的治疗中感到更加满意,未来退出治疗的可能性也会下降。长期以来对患者的社会、认知、生活能力可能有一定的益处,也可能会降低住院率和总体对健保基金的负担,但支持这两点的证据尚且较弱。综述发现现有的研究都发生在高收入国家,所以对于发展中国家的结论也不确定。如果要提供帮助,一般是以认知行为疗法配合低剂量抗精神病药处理psychosis,并提供家庭关系和寻找工作方面的帮助。[145]2013年发表在BMJ的综述认为,早期实施认知行为疗法,可能会降低高风险人士患上精神分裂的风险[146]。英国国家健康与照顾卓越研究院推荐在高风险人士中实施该种疗法[147]
另已知一些药物如大麻、可卡因和安非他命会增加发病风险,不愿得病的人群应避免[19]。
初次出现psychosis的病患可以接受低剂量抗精神病药治疗直到症状缓解,之后继续用药可以预防复发。其中一些人会达成痊愈以至停药也不会复发,但是暂时不清楚怎么识别出这类人。[148]
病情管理
精神分裂症的治疗重心是为患者处方抗精神病药物,一般会在此基础上配合心理及社会支援辅导[9]。当患者严重发作时,可能会自愿地或强制性地住院(如果当地的精神卫生相关法律条文允许强制住院)。长期住院在现在而言是十分罕见的,因为医疗体系从50年代开始去机构化(Deinstitutionalisation),但长期住院的情况现今仍会发生[21]。社区支援服务包括入住康复中心、社区心理健康团队的成员访问、就业能力复康训练[149]。一些证据表明,定期运动对精神分裂症患者的身体和精神健康有一定帮助[150]。截至2015年,穿颅磁刺激对精神分裂症的治疗效果尚不明确[151]。
精神分裂症是中华人民共和国卫生健康委定义的六种严重精神障碍之一(其他五种分别是分裂情感性障碍、偏执性精神病、双相(情感)障碍、癫痫所致精神障碍、精神发育迟滞伴发精神障碍)[152]。

精神分裂症的一线治疗是为患者处方抗精神病药物[153],其可在约7至14天内把阳性症状的程度减轻[153]。然而,抗精神病药物对阴性症状和认知功能障碍的改善效果并不显著[51][154]。若患者持续实行药物治疗,便可降低复发的风险[155][156]。极少证据显示他们实行药物治疗超过两三年后的效果会怎样[156]。然而抗精神病药物可导致患者对多巴胺过敏,增加患者一旦停药后出现症状的机会[157]。
选用抗精神病药物时应考虑它的成效、风险和成本[9]。典型和非典型抗精神病药物之间那种的效果较佳这点至今仍有争议[20][158]。氨磺必利(Amisulpride)、奥氮平(Olanzapine)、利培酮(Risperidone)、氯氮平的效果可能会较佳,但这些药物也与较大的副作用相关[159]。当以低至中等的剂量使用典型抗精神病药物时,其症状复发率和中途放弃率会与非典型抗精神病药物相同[160]。40-50%的个案对药物治疗的应答良好,30-40%的个案在药物治疗后症状部分缓解,治疗抵抗的则有20%(在服用2-3种不同的抗精神病药六周后症状仍没得到令人满意的改善)[51]。氯氮平能有效治疗对其他药物应答差的个案(治疗抵抗性精神分裂症或难治性精神分裂症)[161]。但它在不到4%的人中会导致一种严重的可能副作用——粒细胞缺乏症(低白细胞计数)[19][9][162]。
大多数接受药物治疗的患者都会受到药物的副作用所影响。服用典型抗精神病药物的患者拥有更高的比率出现一种由药物引发的副作用——锥体外综合征,而一些非典型抗精神病药物与体重大幅增加,患上糖尿病及代谢综合征的风险上升相关;这在服用奥氮平的情况下最为明显,利培酮和喹硫平则与体重增加相关[159]。利培酮与氟哌啶醇这两种药物引起锥体外综合征的比率类似[159]。目前尚不清楚新一代的抗精神病药物能否降低诱发抗精神药物恶性综合征或迟发性运动障碍(罕见但严重的神经性障碍)的机会[163]。
针对不愿意或不能定期服用药物的患者,可以使用长效抗精神病药物控制病情[164]。与口服药物相比,长效抗精神病药物能以更大的程度去降低复发的风险[155]。当与心理社会一同介入时,它们可能会改善患者对治疗的长期依从性[164]。美国精神医学学会建议,若患者一年以上没出现任何与精神分裂症有关的症状,则可考虑停药[156]。
除了针对多巴胺系统之外,SEP-363856是近年研究发现能够针对TAAR1跟血清素1A受器的抗精神分裂药物。SEP-363856在研究中能够降低阴性症状,以及改善睡眠状况。[165]
复方药呫诺美林/曲司氯铵(Cobenfy,考本菲)于2024年9月在美国获准用于医疗用途。[166][167] 这是美国美国食品药品监督管理局批准的首个用于治疗精神分裂症的胆碱能激动剂。[166]呫诺美林这个药原来的目的是治疗老年痴呆,但发现除了智力之外对患者的psychosis也大有帮助,尝试在精神分裂症患者身上使用后发现效果不错,[168]只是全身的胆碱能副作用难以接受。后来发现加入不过血脑屏障的抗胆碱能药物曲司氯铵可以抵消,经过几轮临床实验遂成。[169]
许多社会心理介入手段可能有助于治疗精神分裂症,包括家庭治疗[170]、积极性社区治疗、就业协助、认知矫正治疗[171]、技能培训、 代币制治疗,以及针对物质使用和体重管理的社会心理介入[172]。家庭治疗或教育能解决患者的家庭问题,这样可能会减少患者复发和住院的机会[170]。极少证据显示认知行为疗法(CBT)在预防复发或减轻复发的症状这方面是有效的[173][174]。后设认知训练的证据结果不一,一些综述的结论认为其能产生益处,一些则认为不能[175][176][177]。没有较佳质量的研究支持艺术或戏剧治疗的有效性[178][179]。当与正常治疗配合时,音乐疗法能改善精神状态和社会功能[180]。
预后

| 无数据 ≤ 185 185–197 197–207 207–218 218–229 229–240 | 240–251 251–262 262–273 273–284 284–295 ≥ 295 |
精神分裂症花费了庞大的人力和经济成本[9]。它会使患者的预期寿命降低10-25年[8]。这主要是因为它与肥胖、饮食不良、坐式生活型态以及吸烟有关,使患者自杀率和发生意外的状况显著提高[9][8][181]。抗精神病药物也可能有降低预期寿命的风险[8]。精神分裂患者的死亡率一般较非患者高。在一项系统综述(Systematic Review)研究中,发现精神分裂患者和非患者间,死亡率的差异有逐渐增加的趋势[182]。
精神分裂症是身心障碍的主要原因之一,精神分裂是排在四肢瘫痪和痴呆之后第三常见的身心障碍,并比截瘫和失明常见[183]。大约四分之三的精神分裂症患者伴有其他持续性复发的身心障碍[51]。全球有1670万名患者被认为患有中度或重度的身心障碍[184]。有些患者能完全康复及使其他社会功能维持良好状态[185]。大多数精神分裂症患者在社区支持下独立生活[9]。约85%的患者失业[3]。在第一次精神分裂发作的人中,42%的患者有良好的长期预后结果;预后结果一般的有35%;预后结果不佳的则有27%[186]。有研究显示发展中国家的预后结果会比发达国家更好[187],但这项结论备受质疑[188][189]。
精神分裂症患者的自杀率高于平均水平。据引证为10%,但是一项较以上引证新的分析将估计值修改成4.9%,自杀最常发生在发病或首次住院后的一段时间[25][190]。20%至40%的患者至少尝试自杀一次[5][191]。有着各种各样的自杀高危因子,包括患者是男性、伴发抑鬱症和拥有高智商这些特点[191]。
全世界的研究都显示,精神分裂症和吸烟之间拥有着强烈的关系[192][193]。在诊断出精神分裂症的人中,抽烟的比例较一般人口高:普通人群中只有20%是经常抽烟者,精神分裂症患者中则估计达80%至90%[193]。他们更倾向于大量地抽烟,以及抽具有高尼古丁含量的香烟[194]。一些证据表明偏执型精神分裂症患者在独立生活和职业功能上,可能比患上其他类型的精神分裂症的人更为有展望[195]。精神分裂症患者使用大麻的情况亦颇为常见[90]。
流行病学

0-0
1-1
2-2
3-3
4-6
7-20
全世界约有0.3-0.7%人口[9]——相当于2019年全世界约2000万人[22]——在其一生中受精神分裂症所影响。男性的发生率比女性高1.4倍,亦通常较早病发[19](发病的高峰年龄男性25岁,女性27岁[196])。童年发病的患者较为罕见[197],罕见的程度和中年或老年发病者相当[198]。
虽然以前认为精神分裂症在世界各地的发生率差不多,但事实上其发生率在世界各地[5][199]、各国家[200]以及各地区[201]都有不同。估计相差可达五倍[3]。全球失能调整生命年中的约1%是由它所导致[19],它亦在2010年令20,000人死亡[202]。对精神分裂症的定义不同这一点,可使其发生率相差达三倍[9]。
2000年,世界卫生组织发现,受精神分裂症影响的人口百分比和每年的新病例数在全世界大致相同。经过年龄标准化后,每10万男性的患病率:最低为非洲(343人),最高为大洋洲和日本(544人);每10万女性的患病率:最低亦为非洲(378人),最高为东南欧(527人)[203]。在美国,大约1.1%的成年人患有精神分裂症[204]。
历史

在20世纪初,精神病学家库尔特·施奈德把一些他认为能使精神分裂症与其他精神障碍区分的症状列出。这些症状后来称为“首级症状”(first-rank symptoms)或“施耐德主要症状”(Schneider's first-rank symptoms)。当中包括外源所控制的妄想、思想抽离、思想插入、思想广播、听见评论自己的思想或行为的幻听,或能与幻听沟通[205]。虽然施耐德主要症状对当前的诊断标准有很大的贡献,但其特异性仍受到质疑。一份对1970年至2005年间进行的诊断研究回顾发现,施耐德的声称应不需再确认或受到反对,并且建议在未来所修订的诊断系统中应强调施耐德主要症状[206]。缺少施耐德主要症状的患者亦应怀疑其是否真的患上精神分裂症[36]。
精神分裂症的历史具有一定复杂性,且不容易利用线性叙事的方式展述[207]。虽然类精神分裂症在19世纪以前的历史记录中是较为罕见的,但不合理、不可理解或不受控制的行为记录则较为常见。1797年关于詹姆斯·蒂利·马修斯的病例详细报告,以及菲利普·皮内尔于1809年所发表的报告,一般认为是在医学和精神病学文献中最早出现的精神分裂症个案[208]。1886年,德国精神病学家海因里希·舒勒(Heinrich Schule)首次使用拉丁文用语“dementia praecox”(早发痴呆)这一术语去称呼现在的精神分裂症。其后阿诺德·皮克于1891年在他的精神障碍病例报告中使用了它。1893年,埃米尔·克雷佩林借用了皮克和舒勒所使用的术语,并于1899年在精神疾病分类中区分了早发痴呆和情绪障碍(躁狂抑鬱症,包括单相性和双相性抑鬱症)[209]。他认为早发痴呆可能是由长期系统性的疾病或全人疾病所引起的,其影响身体的许多器官和周围神经,但其最终会于青春期后在一连串决定性的事件中影响大脑[210]。他亦利用了“praecox”(早发的)这一术语去把其与其他形式的痴呆如阿尔茨海默病作区分,阿尔茨海默病通常在年老的人身上发生[211]。有时大众会认为1852年法国医生班尼迪克·莫莱尔(Bénédict Morel)使用“démenceprécoce”这一术语可视同医学上对精神分裂症的发现,然而,这项想法忽略了一个事实:在十九世纪末,没有什么可以把莫莱尔所使用的描述性术语跟早发痴呆的独立病发这一概念联系起来[212]。

“Schizophrenia”一词可以直译作“分裂的心智”,它的希腊词根是schizein(撕裂)和phren(心智)[213],以往中国大陆、台湾和香港的名称“精神分裂症”皆是直译此而来[28],台湾后来则改称为“思觉失调症”[29]。欧根·布洛伊勒于1908年第一次提出了这个概念,用来描述人格、思想、记忆、知觉之间的功能分离。美国人和英国人把布洛伊勒的宣称理解成他在形容精神分裂症的“4A”症状:情绪淡然(flattened Affect)、自闭(Autism)、联想障碍(impaired Association)、情感矛盾(Ambivalence)[26][214]。 布洛伊勒意识到这一种疾病并不是痴呆,因为他的一些患者的病情是在改善,而不是恶化,因此提议以“Schizophrenia”称呼这一疾病。在50年代中期,因氯丙嗪的研发和引入,而使精神分裂症的治疗彻底改变[215]。
在20世纪70年代初,精神分裂症的诊断标准出现了不少争议,最终修订成现今所使用的标准。1971年美英诊断学大会发现美国的精神分裂症患者要比欧洲多很多[216],部分是因为美国使用的DSM-II诊断标准比起欧洲的ICD-9更为宽松。大卫·罗森汉于1972年进行并于《科学》期刊发表的著名研究——《精神病房里的正常人》(On being sane in insane places),指出美国的精神分裂症诊断标准往往过于主观且不可靠[217]。这项研究不仅使精神分裂症的诊断标准得以修正,还令整本DSM手册得以修订,使得美国精神医学学会于1980年时出版DSM-III[218]。
“精神分裂症”这一用语通常误解成受其影响的人拥有“多重的人格”。虽然一些诊断出精神分裂症的人可能会听见不存在的声音,并把其视为独特的人格,但精神分裂症并不牵涉到在多个人格中转换。这一种混淆的想法部分可归因于布洛伊勒的用语“精神分裂症”的字面解释(布洛伊勒最初将精神分裂症与分离障碍状联系 起来,并且在他的精神分裂症分类中包含人格分裂)[219][220]。在DSM-II中,解离性人格障碍也常常误诊成精神分裂症,因为其标准诊断较为宽松[220][221]。第一位已知误用该词的人是一名叫托马斯·斯特恩斯·艾略特的诗人,在他于1933年所写的文章中误用“人格分裂”一词[222]。其他学者则追溯到更早的误用根源[223]。
社会和文化

2002年,日本把这一种疾病的名称由“精神分裂病 seishin-bunretsu-byō”改名为“統合失調症 tōgō-shitchō-shō”,以减少疾病名称所带来的社会污名[224],此一名字的灵感是来自生物-心理-社会模型的,且在实行三年内把接受诊断的人数从37%增加到70%[225]。2012年在韩国亦发生了类似的变化[226]。2014年,中华民国卫生福利部宣布将“精神分裂症”正式更名为“思觉失调症”[29],此一名称是考虑到此疾病的核心表现性质——“思考”及“知觉”[227]。精神病学教授吉姆·范·奥斯则建议把英语的“Schizophrenia”(精神分裂症)改名为“psychosis spectrum syndrome”(精神分裂类群障碍)[228]。
在2002年的美国,精神分裂症的耗用成本估计为627亿美元,当中计算了直接成本(门诊、住院、药物和长期护理)和非医疗保健成本(执法、生产率下降和失业)[229]。《美丽心灵》(“A Beautiful Mind”,另译成《美丽境界》)是一部描写约翰·福布斯·纳什(John Forbes Nash Jr.)的生平电影以及书籍:他是一名罹患精神分裂症的诺贝尔经济学奖得主[230]。有“中国的梵高”之称的沙耆亦同样是精神分裂症患者,但他在发病之后仍在藜斋不停画画,其后他的画作受画坛赏识,在1980年代一幅画作的价格更高达数万人民币[231]。
患有严重精神疾病的人受到暴力或非暴力对待的风险会显著增加,包括患有精神分裂症[232]。精神分裂症亦与较常使用暴力有关,但这主要是因为患者的吸毒率较高[233]。与精神病相关的凶杀率类似于与物质滥用相关的,且在一个地区内比例会差不多[234]。若把精神分裂症跟物质滥用分开看待后,其在使用暴力上扮演了什么角色仍是具一定争议性,但个人经历或精神状态的某些层面可能是使用暴力的其中一些因素[235]。约11%服刑中的凶杀者患有精神分裂症,21%的人则患有情绪障碍[236]。另一项研究发现,在研究进行的前一年内,约8-10%的精神分裂症患者对他人行使了暴力,而普通人口的比例则为2%[236]。
与患者行使暴力相关的报导加强了公众认知中精神分裂症与暴力的联系[233]。一项在1999年进行的大型调查显示,12.8%的美国人认为精神分裂症患者“很有可能”对他人行使暴力,48.1%的人则表示他们“有一点可能”会这样做。超过74%的人说患者“不太能”或“不能全部地”作出与治疗有关的决定,70.2%的人说金钱管理上的决定亦如是[237]。根据一项荟萃分析显示,自1950年代以来,行使暴力的精神病患者已经上升了不止一倍[238]。
研究方向
初步研究证实,米诺环素对患者病情的改善有一些效果[239]。亦有关于硝化疗法及努力改善患者的生活环境的研究,用以改善他们能力上的缺陷;然而目前为止还没有足够的证据去对其有效性作出结论[240]。研究人员已证实阴性症状是会对治疗产生挑战,因为它们通常不能通过药物治疗改善。他们亦因此对各种药剂进行了研究,以确定它们可能带来的效果[241],并基于在病理学上,炎症可能对精神分裂症起了一定作用,所以已有针对拥有抗炎活性的药物的研究[242]。
参考文献
参见
外部链接
Wikiwand - on
Seamless Wikipedia browsing. On steroids.
Remove ads