热门问题
时间线
聊天
视角
喝酒的长期影响
饮酒对健康的影响 来自维基百科,自由的百科全书
Remove ads
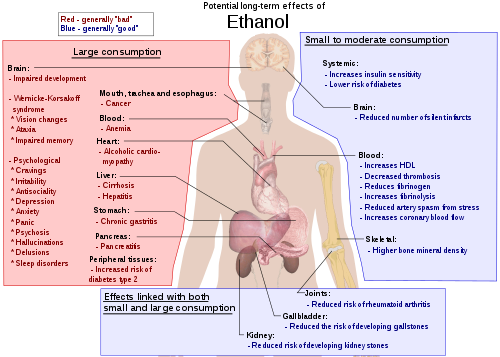
大量饮用乙醇(滥用酒精)会引发严重的有害后果[1]。喝酒的长期影响(英语:Long-term effects of alcohol)包括导致在酗酒、营养不良、慢性胰脏炎、酒精性肝病(简称为ALD)、和癌症方面的增加风险(请参考饮酒与健康)。此外,长期滥用酒精还会损害中枢神经系统和周围神经系统。即使少量和适量的饮酒也会增加罹患类似癌症的风险。[2][3][4][5]
长期饮酒会损害人体的几乎每个器官和系统。[6] 发育中的青少年的大脑特别容易受到酒精毒性的影响。[7] 此外,发育中的胎儿大脑也很脆弱,如果孕妇喝酒,可能会导致胎儿酒精综合症(简称为FASD)。
在西方文化中,人们在100多年前即发现饮酒与心血管疾病之间存有逆关系。[8] 许多医生不提倡饮酒。但是,鉴于酒精相关的许多健康问题,有人建议将酒精视为一种娱乐性药物,应该提倡透过运动和良好的营养以防止心血管疾病。[9][10] 在2013年,酒精性肝病在爱尔兰所有慢性病的比率中,占有五分之四。[11]
酒精相关的负面影响包括增加肝脏疾病、咽癌、食道癌、和胰脏炎的风险。相反,适量饮酒可能对胃炎和胆结石有些益处。[12] 长期不当饮用和滥用酒精会严重影响身心健康。长期过量饮酒,或酒精依赖,会导致神经精神病或神经内科系统疾病、心血管疾病、肝病、和恶性肿瘤。与酗酒有关的精神疾病包括重度抑郁、持续性抑郁症、人格解体、燥郁症、轻度燥郁症、恐慌症、恐惧症、广泛性焦虑症、人格障碍、思觉失调、自杀、神经系统缺陷(例如工作记忆、情绪、管控功能、视觉空间能力、步态与平衡)、和脑损伤。酒精依赖与高血压、冠状动脉疾病和缺血性中风(ischemic stroke)、呼吸系统癌症以及消化系统癌症、肝癌、乳癌、和卵巢癌有关。大量饮酒与肝病,例如肝硬化有关。[13] 过量饮酒可能会有加速衰老的负面影响(参考酒精对老化的影响)。[14]
一些国家推出酒类包装警语,告知消费者有关酒精和癌症,以及孕妇饮酒会导致胎儿酒精综合症的风险。[15]
Remove ads
死亡率效应
一项在2016年所做的系统评价和整合分析发现,在乙醇消费方面,与终生禁酒的人相比,适当的消费不会延长寿命。[16]在疾病对全球负担(Global Burden of Disease)的研究数据所做的系统分析发现,乙醇的摄取会增加罹患癌症的风险,并提高全因死亡率的风险,结论是,让疾病数量达到最小化的乙醇摄取量,是零饮用。[17]
一些研究所得的结论是,少量饮酒(在女性,饮酒少于一份,在男性,饮酒少于两份)与“降低”心血管疾病、中风、糖尿病、和早期死亡的风险有关。[18][19] 其中一些研究把以前曾是酒精饮用者和终生禁酒者都归为非饮酒者的一类,而把终生禁酒对健康有益的好处给遮盖住。喝酒多过前述的少量饮酒的建议,实际上会增加罹患心血管疾病、高血压、心房颤动、还有中风的风险[19]。暴饮可能会导致暴力或意外事故的发生,对年轻人的风险更大[19]。据信,每年约有330万人的死亡可归咎于酒精(占所有死亡人数的5.9%)。[19]
Remove ads
建议每次最大摄入量
不同的国家有不同的建议最大摄入量。在英国,首席医疗官员建议男女每周喝酒不超过14单位(份)。[21][注解 1]。在大多数国家/地区,男子的建议最大数量为每周140-210公克。对于女性,范围是每周84–140公克。(请参考各国建议摄取酒精最大数量)大多数国家建议在妇女怀孕和哺乳期间完全戒酒。
在2018年,《刺胳针》上曾发表大规模讨论,但得出了互相矛盾的结果。一篇报导说"安全"饮酒的上限为每周最多7个"标准单位"的酒精饮料,相当于每周100公克纯酒精。[22] 另一篇的结论是,没有所谓安全的酒精水平,"危害健康最小化的消费水平就是不喝酒",并强调有必要在全世界修订酒精管制政策,以减少总体的酒精消费。[17][23][24]
Remove ads
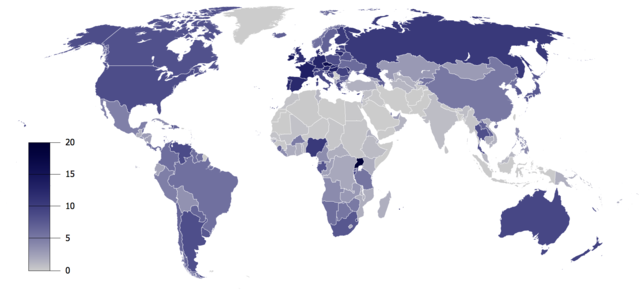
与酒精有关的死亡
无资料
少于50
50–150
150–250
250–350
350–450
450–550
550–650
650–750
750–850
850–950
950–1050
超过1050
过量饮酒在世界上造成许多死亡。研究发现,饮酒导致的总死亡人数与缺乏运动的影响相似。[25] 在2009年的一项评论说,"饮酒对健康的净影响是有害的,据估计,因饮酒而死亡占全球所有死亡人数的3.8%,占全球失能调整生命年(除死亡之外,还加上因为健康状况不佳或失能而损失的‘健康’年岁)的4.6%"。[26]
对西方饮酒文化的研究表明轻度至中度饮酒可能提高相关的存活率。[19][27]有一项针对12,000名,年龄在48-78岁之间的英国男性医生进行的为期23年的前瞻性研究发现,即使把以前饮酒,但后来戒酒者并入目前的饮酒者,再和禁酒者作比较,目前饮酒者的总死亡率仍然比禁酒者低得多。这种益处在缺血性心脏病中最明显,并在其他的血管疾病和呼吸系统疾病中也有体现。“因酒精而获得的”疾病,如肝病和口腔癌,在饮酒者死亡率中占比较大,而由心血管和呼吸系统疾病导致的死亡率,相比之下则不算高。每周摄取8至14个'单位'时,死亡率最低。在英国,1“单位”为10毫升或8公克纯酒精。[28]
较高的摄取量会增加总死亡率,但没有超过禁酒者的对照组。[29]其他研究发现,低度至中度饮酒所导致年龄相关的死亡风险:16-34岁的个体风险增加(由于罹患癌症、意外事故、肝病、和其他因素的风险增加),对55岁以上的人,风险则降低(由于较低的缺血性心脏病发生率)。[30]
这与其他研究所得的结论一致,研究发现中老年男性的饮酒量与总死亡率之间存在J型曲线相关性。以前饮酒,但后来戒酒者,和重度饮酒者的死亡率显著提高,但中度饮酒者的全因死亡率可能降低15-18%。不同国家和地区之间饮酒的定义不同,但这项整合分析发现,低酒精摄取量(女性每天饮酒1-2份,男性每天2-4份)的死亡率低于禁酒的人。[31]
另一项研究[32][33]则对这种结论提出质疑,该项研究发现,在某些品质不高的研究中,把偶尔喝酒,或从前喝酒,后来戒酒的人,归类成为禁酒的人,从而导致这一类人群的死亡率增加。但是,把上述混杂因素排除后做的研究,再次证实全因死亡率和心血管疾病死亡率(CHD mortality)会产生J型曲线。[34][35][36][37]似乎从来没有人讨论过,那些被归类为禁酒的人中,有多少比例的人已经因慢性病而处于较高的死亡风险中,并且由于健康或与药物会产生有害反应的原因,才不饮酒,或者不能饮酒。
观察到的轻度至中度饮酒者,与禁酒者比较而有较低的死亡率,可能部分原因是由于饮酒者有较好的健康状况和较高的社会地位所致;[38] 然而,即使把这些混杂因素调整之后,饮酒对于轻度至中度饮酒者提所供的保护作用仍然显著。[35][37]此外,类似少报酒精摄取量等混杂因素,可能会导致把轻度至中度饮酒者的死亡率低估。[34][39]
在2010年所做的一项研究,证实适度饮酒对死亡率有好的影响。[37]将受测试者分为禁酒者、轻度、中度、和重度饮酒者。死亡率从最低到最高的顺序为中度、轻度、重度、和禁酒者。禁酒者的死亡率风险增加是中度饮酒者的两倍。这项研究专门寻求控制那些混杂因素,包括把以前饮酒,但后来戒酒者被视为非饮酒者的问题。[37]根据另一项研究,酒精摄取量大的饮酒者(一次喝六份或更多),比饮酒摄取量小的人,全因死亡率高出57%。[40] 年轻的禁酒者死亡率最低,年轻的重度饮酒者死亡率最高。[41]
根据2018年的一项研究,每周喝酒超过7份标准量,最多喝到14份标准量的人,预期寿命可能会缩短6个月左右。那些每周喝酒超过14份且最多喝到25份的人,其预期寿命可能会缩短1-2年,而每周喝酒超过25份的,则会缩短4-5年。[22]
与西方文化的研究相比较,在其他文化中的研究则得到相反的结果。著名的INTERHEART Study所做的研究,南亚人的饮酒并不能预防心血管疾病,和其他地区人口因喝酒而有益处的结果有鲜明的对比。[42]实际上,饮酒的亚洲印度人在心脏病发作的风险高出60%(其中喝本地烈酒的占80%,而喝有品牌烈酒的占50%)。[43]在归类为偶尔,和经常的轻度、中度、和重度饮酒者中都发现有这种危害。[43]
在印度,针对4,465名受测试者所进行的另一项大型研究也证实,饮酒会产生对男性心血管疾病的危害。与禁酒者相比,饮酒者的血糖高出2mg/dl(2毫克/升),血压高出2mmHg(2毫米汞柱),和高密度脂蛋白胆固醇高出(2mg/dl)(2毫克/升),这类人吸烟的比率也比禁酒的人高得多(63%比21%)。[43]
Remove ads
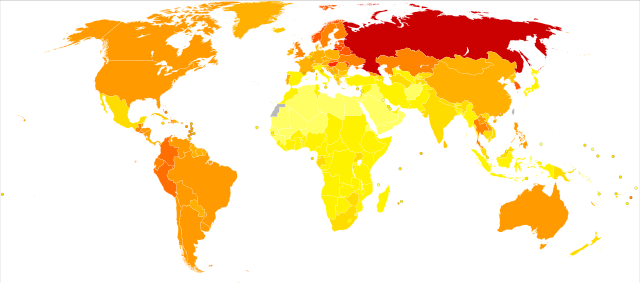
一项研究声称,"近年来,俄罗斯人过度饮酒,尤其是男性,占年龄层在15-54岁之间死亡人数的一半以上。"[44] 但是,这项研究存有一些难题。例如,同一项研究还发现大量饮酒对乳癌死亡率具有保护作用。这与公认的科学观点相矛盾,即酒精会增加罹患乳癌的风险。[45] 关于这一点,在做进一步沟通讨论之后,得到的建议是"需要对与饮酒有关的死亡率统计数据做仔细的解读,同时要考虑到其他相关的危险因素、发病率、和存活率。"[46]
在英国的一份政府报告中的资料,"在2007年与酒精有关的死亡人数是8,724人,比2006年要低,但比1991年记录的4,144人增加两倍多。与酒精有关的死亡率在2007年为每10万人中有13.3人,1991年每10万人中有6.9人。" [47] 在苏格兰,国民保健署估计在2003年每20人中就有1人的死亡与酒精有关联。[48] 2009年的一份报告指出,与酒精有关的疾病所导致的死亡为9,000人,是25年前的3倍。[49]
英国的一份报告得出的结论是,低度至中度饮酒对死亡率的影响取决于年龄。低度至中度饮酒会增加16-34岁间个人的死亡风险(由于罹患癌症、意外事故、肝病、和其他因素的风险增加),但会降低55岁以上个人的死亡风险(由于缺血性心脏病的风险降低的缘故)。[50] 英国的一项研究发现,酒精在英国所引起的癌症约占全部癌症病例的4%(每年12,500例)。[51]
美国疾病管制与预防中心(简称为CDC)报告:"从 2001年至2005年,每年大约有79,000人死于过量饮酒。事实上,过量饮酒是美国人每年与生活方式相关的第三大死亡原因。"[52]在1993年的一项研究估计,美国因饮酒而死亡的人数为100,000。[53]
CDC在2001年的另一份报告估计,当年在美国,中度和高度饮酒导致75,754人死亡。饮酒量低有一些有益的作用,因此,净死于酒精的人数是59,180人。[54]
寿命
2016年,有项饮酒和死亡风险研究,针对87项案例做整合分析。案例分析后的结果,中度饮酒者死亡率风险降低的最大,但这些研究并未纠正某些定义为禁酒者相关的混淆变数,例如这些人是否有先前的酗酒和慢性健康上的问题。在对这些针对禁酒者变异做调整之后,发现小量饮酒者的死亡率没有降低。[55]然而,另有个别研究显示,对55岁以上的人进行混杂因素调整后,禁酒者和重度饮酒者的死亡率比中度饮酒者的增加约50%。[56]
心血管系统
酒精具有抗凝血作用。[57]中度饮酒者的血栓形成率比禁酒者低。[58]一项对随机试验的整合分析发现,适度饮酒会降低血清纤维蛋白原(一种促进血凝块形成的蛋白质)的水平,同时会增加组织型纤维蛋白溶酶原激活物(一种有助于溶解血凝块的酶)的水平。[59]估计这些变化可将冠状动脉疾病风险降低约24%。2011年的另一项整合分析发现,中度饮酒,会对有关的高密度脂蛋白胆固醇、脂联素、和纤维蛋白原发生有利变化。[60]
根据针对16,351名参与者的系统评价显示,心血管疾病死亡率与饮酒量之间的总体关系以J形曲线呈现。每天饮酒5-10公克有最大的保护作用,到每天饮酒26公克时仍然效果显著。[61]中度饮酒者的血清C反应蛋白(简称为CRP)是炎症和心血管疾病风险的预测指标,其水平低于禁酒者,这表明适度饮酒可能具有抗炎症作用。[62][63][64]一项前瞻性研究的数据显示,在最初饮酒量较低(每周喝酒少于或等于1份的男性)者中,随后适度增加饮酒量,可能会降低他们在心血管疾病的风险。[65]
虽然是有前面说的流行病学上的证据,许多人还是提出不要为了健康而饮酒的建议。世界卫生组织(简称为WHO)的一名医生将这种提倡饮酒的行为标志为"荒谬而危险的"。[66][67]一位评论者指出:"尽管有丰富的观察数据,但因为尚未进行任何随机对照试验,尚无绝对明确的证据表明酒精可降低心血管疾病的风险。不应该建议患者使用酒精去降低心血管疾病的风险,来替代那些已经被充分证实过的方法:如适当的饮食、运动、和药物等。” [68]
有人认为,酒精对健康的好处,纵然说有,但还有争议,而且酒类产业可能把这一观点加以扩大,研究人员认为,酒精应被视为是对健康有潜在严重不利影响的娱乐性药物,不应推广用来对心血管疾病提供保护。[69][70]
Remove ads
在1997年发表的一项前瞻性研究发现,"适度饮酒似乎可以降低看来明显健康的男性罹患周边动脉疾病的风险。"[71]在一项针对人群的大型研究的结果显示,适度饮酒与女性罹患周边动脉疾病成反比,而与男性则无这种现象。但是,当把吸烟这种混淆因素列入考虑时,这种好处就扩展到了男性。这项研究得出的结论是"在不吸烟的男女中,饮酒与周围动脉疾病之间存在负相关的关系。" [72][73]
有一项研究发现,适量饮酒对间歇性跛行有保护作用。对每天喝1至2份酒的男性,和每天喝半份至1份酒的女性,风险最低。[74]
适量饮酒经发现可帮助心脏病发作的人存活。[75][76][77]但是,过量饮酒会增加心脏衰竭的风险。[78]文献评论说,半份酒精饮料提供的保护水平最佳。但是他们指出,目前尚无随机对照试验来证实低剂量酒精对心脏病发作具有保护作用。[79]如果每天服用3份或更多的标准量酒精饮料,则会增加高三酸甘油脂血症、心肌症、高血压、和中风的风险。[80]一项系统评价报告说,依照剂量方式来减少重度饮酒者的摄取量,可降低血压。对于每天喝两份或更少酒的人,则没有发现有差异。[81]
长期摄取大量的酒精会导致酒精性心肌症。酒精性心肌症的临床症状与病因不明扩张型心肌病相同,涉及心脏肌肉组织肥大,可导致心脏衰竭。[82]
神经系统

长期大量饮酒会损害大脑发育,导致酒精相关性失智、脑损伤、身体依赖、酒精性周边神经病变(也称为“酒精腿”,alcohol leg),加剧神经精神方面和认知的障碍,并导致神经化学异常。目前,由于不良的研究设计和方法,关于适度饮酒会增加还是降低失智症的风险,尚无文献给予定论。[85]一些研究提出,低度至中度饮酒对年龄相关的认知能力下降,以及失智症有保护作用。然而,其他研究尚未发现低度至中度饮酒有这种保护作用。[86]
一些证据显示,低度至中度饮酒可能会加速大脑容量的损失。[87]长期饮酒可能导致血浆中有毒氨基酸高半胱氨酸水平升高,[88][89]这可能是酒精戒断症候群发作的原因,[90]酒精引起的脑萎缩[91],以及与酒精相关的认知障碍[92]。酒精对神经系统的影响还包括记忆力和学习障碍(请参阅酒精对记忆的影响),例如导致失忆症现象。
针对中年人群所做的流行病学研究,通常发现饮酒与中风风险之间的关系呈U型或J型曲线的形式。[93][94][95][96] 根据所研究的中风类型,酒精可能会有很不同的影响。在西方文化中,中风的主要形式是缺血性,而在非西方文化中,出血性中风案例则较多。,每天摄入2份以上的酒精饮料与酒精对缺血性中风的有益作用相反,会增加出血性中风的风险。
美国国家中风协会估计,大量酒精摄取酒精会让中风的风险增加50%。[97]"对于中风,在特定人群中观察到的饮酒与危险之间的关系,取决于出血性中风的比例。轻度至中度饮酒可降低缺血性中风的风险,这在一定程度上可能有因果关系。另一方面,出血性中风与饮酒呈对数线性关系。"[98]
酗酒与广泛而严重的大脑损伤有关。与酒精有关的脑部损伤不仅是由于酒精的直接毒性作用所致;而且酒精戒断症候群、营养不良、电解质紊乱、和肝损伤等,也被认为会导致与酒精有关的脑部损伤。[99]
过量饮酒与前瞻性记忆受损有关。这种认知能力的受损,导致日后无法执行未来该做事情的状况会增加,例如,忘记锁门或按时寄信。所摄取的酒精量越高,饮用的时间越长,损害就越严重。[100]对长期饮酒的毒性最敏感的器官之一是大脑。在美国,大约20%的精神病院的入院,都与酒精相关的认知障碍有关,最明显的是酒精相关的失智症。
长期过量饮酒还与严重的认知能力下降,和一系列神经精神科并发症有关。老年人在酒精毒性对大脑的作用最敏感。[101]有一些不确定的证据显示,在成年早期摄取少量酒精,对以后的生活具有保护作用,可防止认知能力下降和失智。[102]然而,一项研究得出的结论是:"我们的发现表明,尽管有先前的建议,但适度饮酒并不能保护老年人免受认知能力下降的影响。"[103]
魏尼克-高沙可夫症候群是维他命B1缺乏的一种表现,通常是酗酒的副作用。[104]该症候群是两种同名疾病的综合表现,即高沙可夫症候群和魏尼克脑病。魏尼克脑病的表现是急性的,其特征是意识模糊,而高沙可夫症候群的主要症状是失忆症和管控功能障碍。[105] 香蕉袋是装有维生素和矿物质(由于维生素而呈亮黄色)的静脉注射液容器,可用于减轻这些后果。[106][107]
通过喝少量的酒精可对原发性颤抖症患者,或者在有原发性颤抖症家族史的背景下,可在发生后短暂缓解患者多达三分之二的症状。[108]
已知乙醇会激活A型γ-氨基丁酸受体(简称为GABAAR)并抑制N-甲基-D-天门冬胺酸受体(简称为NMDA),这些均与原发性颤抖病理有关[109] ,并且可能是改善作用的基础。[110][111] 另外,在不同的动物原发性颤抖症模型中,也做过乙醇作用的研究。(有关此主题的更多详细信息,请参阅“原发性颤抖症”的英文版。)
长期使用酒精来引导睡眠会导致失眠:在睡眠阶段之间频繁变动,会因头痛和流汗而醒来。停止长期酗酒还会导致梦境生动,严重影响睡眠。长期酒精滥用与非快速动眼睡眠第3和4期,以及抑制快速动眼期睡眠,还有快速动眼期睡眠破碎有关。在酒精戒断症候群期间,快速动眼期睡眠的发生,通常被放大称为是快速动眼期睡眠反弹作用的一部分。[112]
大量饮酒者和酗酒者发生严重抑郁症的几率很高。虽有某些证据表明饮酒会导致这种严重抑郁疾病,但是否由抑郁症导致自我用药酒精滥用,还是饮酒引起的酗酒者抑郁症增加,还未有定论。[113]酗酒与许多精神健康疾病相关,同时酗酒者的自杀率很高。[114]一项针对因自杀未遂而住院的人所做的研究显示,酗酒者后续成功自杀的可能性是非酗酒者的75倍。[115]在一般酗酒者人群中,自杀风险比普通人群高5-20倍。大约有15%的酗酒者会自杀。滥用其他药物也会增加自杀的风险。35岁以下的年轻人中约有33%的自杀与酒精或其他物质滥用有关。[116]
由于酒精对大脑,尤其是大脑前额叶皮质区的神经毒性作用,在酗酒的人中社交技能显著受损。受到酗酒损害的社交技能,包括面部表情感知能力、语言韵律感知能力、和心智理论感知能力;酗酒者也无法理解幽默。[117]
研究结果显示,酒精依赖与酒精戒断后的渴望 和易怒直接相关。[118]另一项研究显示,饮酒是导致儿童反社会行为的重要诱因。[119]忧郁症、焦虑症、和恐慌症是酒精依赖者通常罹患的疾病。酗酒与负责处理情绪的大脑网络(例如杏仁核和海马体)的活化减弱有关。[120]长期戒酒之后,精神健康障碍症状的改善或消失,表示这种障碍通常是由于酒精滥用引起的大脑神经化学畸变而引起的,但这障碍问题在戒断初期和恢复期间可能会有恶化的情形。[121][122][123] 思觉失调会发生在几种酒精相关疾病之后,包括急性中毒和大量烂饮之后的戒断时期。[124]与其他滥用药物相比,长期滥用酒精更会导致思觉失调症状的发展。已有证据显示,酗酒会导致男性思觉失调的风险增加800%,女性思觉失调的风险增加300%,而这与先前存在的思觉失调疾病并无关联。这明显高于因使用大麻所产生的结果,让酗酒成为导致思觉失调的非常重大原因。[124]约有3%的酒精依赖者在急性中毒或戒断期间会出现思觉失调的情况。与酒精有关的思觉失调可能会透过药物戒断并发引发机制展现出来。与酒精有关的思觉失调的机制是由于神经元膜变形、基因表现、以及维他命B1缺乏所致。在某些情况下,酗酒,会透过药物戒断并发引发机制,可能会导致慢性药物引发的精神病(即精神分裂症)的发展。与酒精有关的思觉失调的影响包括抑郁和自杀,以及社会心理障碍的风险增加。[124]然而适度的饮酒,显示是可降低罹患抑郁症的风险。[125]
虽然酒精最初会帮助克服社交恐惧症或恐慌症状,但长期滥用酒精经常会加重社交恐惧症的症状,并在酒精中毒期间,尤其是在酒精戒断症候群期间,会导致恐慌症的发展或恶化。这种作用并非只是酒精所独有,但长期使用与酒精具有类似作用的药物(例如苯二氮䓬类药物)也可能发生,苯二氮䓬类药物有时被开立处方,作为有酒精问题的人服用的镇静剂。[126]约有一半因精神焦虑症(如恐慌症或社交恐惧症)而接受精神医疗服务的患者,患有酒精依赖,或苯二氮䓬类药物依赖的问题。应当指出,每个人对酒精或镇定剂,安眠药都有各自的敏感性水平,一个人可忍受而不会生病,而另一个人则会因同样原因而生大病,并且即使只有适度饮酒也会引起反复性症候症和睡眠障碍。遭受酒精毒害的人,将无法从其他疗法或药物中受益,因为它们的根本原因并未解决。[127]
酒精成瘾与迄今为止的任何药物滥用所测试出来的结果都一样,与伏隔核中GLT1(EAAT2)的持续下降有关,并且与所有文献记录里的成瘾综合症中,几乎千篇一律的觅药行为(drug-seeking behavior)有关。麸胺酸传递的长期失调、加上与重新暴露于药物使用而触动情况复发、以及对其他改善药物成瘾的可能性的总体增加,让情况更为不利。目前已有有助于重新稳定谷氨酸系统的药物,例如乙酰半胱氨酸,用于治疗对古柯碱,尼古丁,和酒精成瘾的症状。[128]
消化系统和体重增加
酒精对体重增加的影响是有争议的:一些研究没发现有这样的效果[129],另一些研究则发现对体重有减少[130]或者增加的影响。
在美国进行的一项国民健康与营养检定调查(NHANES)得出的结论是:"轻度至中度饮酒与代谢症候群的患病率较低有关,对脂肪、腰围、和空腹胰岛素产生有利影响。这种关系在白人中,以及喝啤酒及葡萄酒的人最为明显。[132]同样,在韩国进行的一项全国调查显示,酒精摄取与代谢症候群之间存在J形曲线关联:"本研究的结果显示,代谢症候群与轻度饮酒呈负相关(韩国成年人每天饮酒1–15公克)",但在饮酒量大的人,则危险会增加。[133]
研究发现,饮酒可降低胆结石的发生风险。根据年龄、性别、教育程度、吸烟与否、和身高体重指数来分类,和禁酒者做比较,偶尔和经常轻度饮酒者(每天少于25公撮)的胆结石相对风险为0.83,中度饮酒者(每天25-50公撮)为0.67,重度饮酒者为0.58。这种反向关联在年龄、性别、和身高体重指数的各个层次上都是一致。[134]饮酒频率似乎也是一个因素。"饮酒频率的增加也与降低风险有关。结合饮酒量和饮酒频率的报告,反映出任何给定饮酒量(5-7天/周)的频繁摄取的方式与不饮酒者相比,患病风险降低。相比之下,不经常饮酒(1-2天/周)与患病风险没有显著相关性。” [135]
在1998年发表的一项大型自我报告研究发现,胆囊疾病与多种因素(包括吸烟、饮酒、高血压、和喝咖啡)之间没有关联。[136]在1997年所做的一项回溯性研究发现,在饮酒者中使用维生素C(L-抗坏血酸)补充剂与胆囊疾病的患病率较低相关,但在非饮酒者中未发现有这种关联。[137]
酒精性肝病是一种主要的公共卫生问题。例如,在美国有多达200万人患有与酒精有关的肝病。[138]长期酗酒会导致脂肪肝、肝硬化、和酒精性肝炎。治疗选择有限,最重要的就是停止饮酒。碰到严重的肝病,唯一的治疗选择可能是来自禁酒者捐赠的肝脏移植。目前正在研究肿瘤坏死因子抑制剂的有效性。某些补充药物,例如水飞蓟和水飞蓟素,似乎可提供一些效果。[138][139] 酒精是西方世界中导致肝癌的主要原因,占肝癌病例中的32-45%。在美国有多达50万人罹患有与酒精有关的肝癌。[140][141]
酗酒是导致急性胰脏炎和慢性胰脏炎的主要原因。[142][143]酒精性胰脏炎可产生严重的腹痛,并可能发展为胰脏癌。[144]慢性胰脏炎通常会导致肠道吸收不良,并导致糖尿病。[145]
酒精会影响长期饮酒者的营养状况。它会减少食物摄取并导致吸收不良。它会导致骨骼肌质量失衡,并导致肌肉萎缩。长期饮酒还会增加人体中重要蛋白质的分解,从而影响基因表现。[146]
其他系统
长期摄取酒精会损害肺部的多种关键细胞功能。[147]这些细胞损伤可导致因肺部疾病,严重并发症发生的可能性。最近的研究指出,与酗酒导致的肺部疾病相关的死亡,与酒精导致肝病的死亡可相提并论[148],与禁酒者比较,酗酒者罹患急性呼吸窘迫症候群(简称为ARDS)的风险,与因为ARDS而死亡的比率较高[149]。一项大规模的前瞻性研究与这些发现相反,认为适度饮酒对呼吸道疾病导致的死亡具有保护作用。[29]
长期过量饮酒会导致中枢神经系统和周围神经系统受损,导致男性性欲减退和阳痿。[154]这是由于乙醇引起的睾丸萎缩,导致睾丸激素分泌减少,男性的女性化程度提高,也是酗酒男性肝硬化的临床特征。[155]
过量饮酒会导致雌激素过多。[156] 据推测,含酒精的饮料可能含有类似雌激素的化合物。在男性中,高水平的雌激素可导致睾丸功能衰竭,和发展出女性特征,包括男性乳房的发育(男性乳房发育症)。[157][158] 在女性中,由于过量饮酒会导致雌激素水平升高,与乳癌风险增加有关。[158][159]
一项整合分析,以终生禁酒者为参照群,透过性别和指标(end point)来确定剂量-反应之间的关系。分析发现,对于男女两性都呈现U形曲线的关系。与终生禁酒者相比,男性中2型糖尿病的相对风险(简称为RR)在每天饮酒22公克时保护作用最高,而每天饮酒60公克以上时有害。在妇女中,每天饮酒24公克时保护作用最高,每天饮酒约50公克时变得有害。[来源请求]对妇女干预研究的系统评价,所得结果也支持这项发现。报告说,适度饮酒可提高女性的胰岛素敏感性。[160]
饮酒的方式(即进餐时饮用,或是暴饮)会影响各种健康结果[161]。可能的情况是,与大量饮酒有关的糖尿病风险,是由于饮酒主要是在周末一次喝完,而不是在一周内把与前述相同数量的酒分开而平均饮用所引起。[161] 在英国针对暴饮,会"建议避免每周饮用(暴饮)"。[来源请求]来自芬兰的一项为期二十年的相同研究报告显示,适度饮酒可降低男女患2型糖尿病的风险。然而,暴饮和高量饮酒会增加女性2型糖尿病的风险。[162]
经常饮酒与痛风性关节炎风险增加[163][164],和类风湿关节炎风险降低有关。[165][166][167][168][169]最近的两项研究报告说,饮酒越多,罹患类风湿关节炎的风险越低。在经常喝酒的人里面,其中四分之一喝酒最多的人,患病率要比喝酒最少的一半的人,发病机会降低50%。[170]
研究人员指出,适度饮酒还可降低其他发炎(如心血管疾病)的风险。乙醇可通过某些生物学机制降低破坏性关节炎的风险,并防止骨质密度(bone mineral density,BMD)的流失,而骨质密度流失是疾病发展过程的一部分。[171]
一项研究得出的结论是:"或者酒精会预防类风湿关节炎(简称为RA),或者患有RA的受试者会在RA发病后减少饮酒。" [172] 另一项研究发现,"更年期后妇女,平均每周喝酒超过14份的,患类风湿关节炎的风险降低……" [173]
适度饮酒与更年期后的妇女较高的骨质密度有关。 "……饮酒显著把骨质疏松症的可能性降低。" [174] "更年期后年长妇女的适度饮酒与较高的骨质相关。" [175] "[45岁以上]男性和女性的社交饮酒,与较高的骨质密度相关。"[176] 但是,酗酒与骨质流失有关。[177][178]
长期过度饮酒会导致多种皮肤疾病,包括荨麻疹、缓发性皮肤病变紫质症、潮红、肝硬化的皮肤瘢痕、牛皮癣、痒、脂溢性皮炎、和酒糟鼻。[179] 一项在2010年所作的研究得出结论:"喝淡啤酒与女性罹患牛皮癣的风险增加有关。在这项研究中,其他酒精饮料并未增加牛皮癣的风险。" [180]
免疫系统
饮酒可预防主动感染幽门螺杆菌[181]。相比之下,饮酒(每天饮酒超过30公克的人,与不饮酒的人相比)与十二指肠溃疡(请参考胃及十二指肠溃疡)的较高风险无关。[182]酗酒者的过量饮酒是已知的肺炎危险因子。
一项关于普通感冒的研究发现,"大量的酒精饮料(每天最多3到4份)与感冒的风险降低相关,因为饮酒与感染后的生病减少相关。但是,饮酒的好处仅发生在非吸烟者身上。[........]虽然饮酒并没有影响吸烟者患临床疾病的风险,但适度饮酒会降低不吸烟者的风险。"[183]
另一项研究的结论是:"研究结果显示,摄取葡萄酒,尤其是红酒,可能对普通感冒有保护作用。啤酒、烈酒、和酒精摄取总量似乎并不影响到普通感冒的发生。”[183]
癌症
1988年,WHO的国际癌症研究机构把酒精列为一类致癌物,这个机构说:"有充分的证据证明酒精性饮料对人体的致癌性……酒精性饮料对人类具有致癌性(第1类)。" [184] 美国卫生与公共服务部的国家毒理学计划在2000年把酒精列为“已知的致癌物质”。[185]
据估计,2006年"全世界中有3.6%的癌症病例与饮酒有关,因此导致的死亡占所有癌症死亡的3.5%。" [186]在2011年所做的一项欧洲研究发现,男性癌症的10分之1,与女性癌症的33分之1,是由于过去或现在的酒精摄取所引起。[187][188]世界癌症研究基金会小组的报告《“食物、营养、体育活动、和癌症预防:全球视野”》发现 "有说服力"的证据,显示酒精饮料会增加以下癌症的风险:嘴巴、咽和喉、食道、大肠癌(男性)、乳癌(更年期前后)。[189]
即使少量和中度饮酒也会增加个人的癌症风险,尤其是在食道鳞状细胞癌(请参考食道癌的英文版)、口咽癌、和乳癌。[190][191]
乙醛是酒精的代谢产物,被怀疑会导致癌症。[192]通常,肝脏会把饮酒所产生的乙醛消除掉99%。但是,肝脏疾病和某些遗传酶缺乏症会导致乙醛水平升高。已发现在重度饮酒者,由于酒精醇脱氢酶的遗传缺陷,而暴露在高乙醛水平,罹患上消化道和肝脏癌症的风险更大。[193]在2007年所做的一项审查发现"有说服力的证据表明,乙醛...让乙醇发生致癌作用,是由于乙醛对脱氧核糖核酸(DNA)的多种促使突变作用。" [194]乙醛可与DNA反应生成包括Cr-PdG在内的DNA加合物。这种Cr-PdG加合物"可能在酒精饮料相关的致癌机制中发挥重要作用。"[195]
酒精对胎儿的影响
胎儿酒精综合症(即胎儿酒精谱系障碍,或称FAS,Fetal alcohol syndrome)是先天性障碍,发生在怀孕期间饮酒的妇女后代中。根据对当前知识的调查,怀孕妇女饮酒风险多于收益。[196]酒精会穿过胎盘屏障,阻碍胎儿的成长或体重,造成独特的面部瘢痕,损害神经元和大脑结构,并引起其他身体、精神、或行为问题。[197]
胎儿接触酒精是西方世界里面,导致智力障碍的主要原因。[198]怀孕期间饮酒,与脑胰岛素抗性和类胰岛素抗性的生长因素有关。[177]
酗酒对家庭和儿童的长期影响
在酗酒家庭中长大的孩子,在涉入自己的固定情感关系时,有可能会遭受情绪上的困扰。这种孩子在离婚和分居、婚姻状况不稳定、和家庭破裂方面,有较高的风险。[199]儿童时期经历的抑郁和反社会行为的情绪,经常导致婚姻冲突和家庭暴力。妇女比男子更有可能成为与酒精有关的家庭暴力的受害者。[200][201][202][203]
酗酒者的子女,经常将从孩子时期中学到的行为,纳入他们自己的婚姻关系中。这些行为导致不良的养育做法。例如,酗酒者的孩子成年后,可能同时会对孩子或配偶表达爱和摈弃。这称为不安全型依附(insecure attachment,请参考依附理论中安全型依附)。[199][202][203]不安全型依附会导致与亲密伴侣和后代在信任和联系上发生问题。此外,先前的父母缺乏情感上的支持,会导致子女长大后,在成人关系中,缺乏解决冲突的技能。[199]证据显示,酗酒的父亲表现出苛刻和无效的养育做法,与青少年和成年人的酒精依赖有关。 [202][203]
酗酒者的子女由于害怕被遗弃而常常无法信任其他成年人。[199] 此外,由于孩子们通过观看父母的互动来学习他们的交往行为,因此,有酗酒父亲的女儿成年后可能无法与男人适当地互动。[199]酗酒父母的不良行为榜样导致对如何进行异性互动的认识不足。[199]
酗酒者的儿子面临自我调节不良的风险,这种情况经常在学龄前就表现出来。这导致他们将自己行为的问题,和无法控制冲动都归咎于他人。不良的决策,特别是在酗酒者的儿子中,与他们早期就开始饮酒有关。[200][201][203]儿子经常表现出寻求刺激的行为,避免受伤害,并且表现出忍受挫败能力不足的情况。[201][202][203]
健康风险和饮酒
有许多短期和长期的健康状况可归因于饮酒。有完整的记录显示,长期让自己处在有害状况下,其中一些状况会让几个重要器官永久受损,很难治疗。在这些情况中,来自一种或多种因素,最终的结果就是造成死亡。据报告,在2006年至2010年之间,由于过度饮酒在美国有88,000人因此死亡。[204]
医生通常认为饮酒是让几种慢性病变得更难治疗的直接原因,因此建议少次,少量饮酒,以防止进一步让破坏性损害发生。一些医生强烈建议戒酒,以预防心脏病、脑损伤、和肝病。
性功能 众人皆知长期使用酒精会损害神经系统、心脏、肝脏、和生殖器官,导致成年男性性能力下降。此外,由于有长期饮酒精相关的精神障碍,可能会导致倾向进行无保护的性行为,和与多伴侣的性行为。这情况可能会导致曝露在性传染病的风险,以及意外怀孕。[205]
对胎儿的影响 在怀孕期间仍继续饮酒的妇女,极有可能生下有缺陷的后代。由于酒精能够透过母亲传递给婴儿的营养,直接传到胎盘,因此对胎儿的发育直接发生影响,导致细胞受损、先天缺陷、神经系统疾病、还有流产。[206]
对重要器官的影响 研究结果显示,大量饮酒与器官损害之间存在着破坏性关系。心血管的问题,如高血压、心肌病、和心脏病等,可归因于过量饮酒。除循环系统之外,肾脏和肝脏疾病也可归因于饮酒。也有对大脑功能的影响,例如记忆力减退而降低智力,大脑容量和协调能力的损失。[207]
社交能力影响 长期过度使用酒精会导致许多难以治疗的状况,例如抑郁、冲动性决策、暴力、虐待行为、和认知能力下降。所有这些都会降低与家人,朋友互动的品质,并可能会导致对自己和他人做出有害的行为。[208]
长期饮酒对经济的影响
当前没有一致的方法来衡量饮酒在经济上的影响。[209]疾病的直接、间接、和无形成本等在经济上的负担,可透过过疾病成本的研究来进行估算。[210]直接成本是对患病率和发病率研究来估算,而间接成本是通过人力资本方法、人口学方法、和摩擦成本(friction cost)方法估算的。[209] 但是,由于使用方法、与酒精消费有关的成本项目、和衡量技术的差异,经济影响很难准确地被衡量。
酒精依赖对健康结果有深远的影响。2016年在德国进行的一项研究发现,有酒精依赖问题的人产生的经济负担比没有的人高出 50%。[211]在这项研究中,一半以上的经济成本是由于生产力损失所造成,而只有 6%是由于对酒精问题做治疗所致。这种经济成本主要由30至49岁之间的人来承担。在另一项根据来自8个欧洲国家的数据所做的研究中,[212]77%的酒精依赖患者患有精神病和躯体合并症(somatic comorbidity),从而增加医疗卫生和经济上的成本。饮酒还会影响免疫系统,并在罹患艾滋病、肺炎、和结核病的人身上引起并发症。[213]
因酒精依赖而产生的间接成本非常巨大。最大的间接成本来自生产力损失,其次是过早死亡。[214]在美国,酒精依赖的男性劳动力参与率降低2.5%,收入的降低达到5.0%,缺勤率增加 0.5-1.2天。女性酗酒者的缺勤率则增加0.4-0.9天。过早死亡是酒精依赖间接成本的另一个重要因素。[215]在2004年,全球死亡人数中有3.8%与酒精有关(男性为6.3%,女性为1.1%)。60岁以下的人在全球因酒精导致的死亡人数中,比率更高,为5.3%。
一般而言,间接成本,例如因酒精依赖而导致的过早死亡,由于旷工旷职所引起,和导致出工者的生产力下降、财产损失、和执法成本,都远远超过直接医疗卫生和执法成本。[216] 汇总来自各方面所有的经济成本,其影响可能占一个国家国内生产总值(GDP)的0.45%至5.44%。[217]估计数字差距大的原因是由于对经济负担的衡量方法不一致,因为有些研究人员将长期饮酒可能带来的正面影响,列入衡量之中[217][218][219]。
参见
参考文献
注解
外部链接
Wikiwand - on
Seamless Wikipedia browsing. On steroids.
Remove ads