Corticosteroid
Class of steroid hormones From Wikipedia, the free encyclopedia
Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex of vertebrates, as well as the synthetic analogues of these hormones. Two main classes of corticosteroids, glucocorticoids and mineralocorticoids, are involved in a wide range of physiological processes, including stress response, immune response, and regulation of inflammation, carbohydrate metabolism, protein catabolism, blood electrolyte levels, and behavior.[1]
| Corticosteroid | |
|---|---|
| Drug class | |
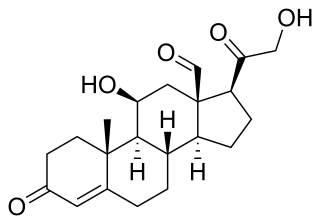
 Cortisol (hydrocortisone), a corticosteroid with both glucocorticoid and mineralocorticoid activity and effects. | |
| Class identifiers | |
| Synonyms | Corticoid |
| Use | Various |
| ATC code | H02 |
| Biological target | Glucocorticoid receptor, Mineralocorticoid receptor |
| Chemical class | Steroids |
| Legal status | |
| In Wikidata | |
Some common naturally occurring steroid hormones are cortisol (C
21H
30O
5), corticosterone (C
21H
30O
4), cortisone (C
21H
28O
5) and aldosterone (C
21H
28O
5) (cortisone and aldosterone are isomers). The main corticosteroids produced by the adrenal cortex are cortisol and aldosterone.[1]
The etymology of the cortico- part of the name refers to the adrenal cortex, which makes these steroid hormones. Thus a corticosteroid is a "cortex steroid".[citation needed]
Classes



- Glucocorticoids such as cortisol affect carbohydrate, fat, and protein metabolism, and have anti-inflammatory, immunosuppressive, anti-proliferative, and vasoconstrictive effects.[2] Anti-inflammatory effects are mediated by blocking the action of inflammatory mediators (transrepression) and inducing anti-inflammatory mediators (transactivation).[2] Immunosuppressive effects are mediated by suppressing delayed hypersensitivity reactions by direct action on T-lymphocytes.[2] Anti-proliferative effects are mediated by inhibition of DNA synthesis and epidermal cell turnover.[2] Vasoconstrictive effects are mediated by inhibiting the action of inflammatory mediators such as histamine.[2]
- Mineralocorticoids such as aldosterone are primarily involved in the regulation of electrolyte and water balance by modulating ion transport in the epithelial cells of the renal tubules of the kidney.[2]
Medical uses
Summarize
Perspective
Synthetic pharmaceutical drugs with corticosteroid-like effects are used in a variety of conditions, ranging from hematological neoplasms[3] to brain tumors or skin diseases. Dexamethasone and its derivatives are almost pure glucocorticoids, while prednisone and its derivatives have some mineralocorticoid action in addition to the glucocorticoid effect. Fludrocortisone (Florinef) is a synthetic mineralocorticoid. Hydrocortisone (cortisol) is typically used for replacement therapy, e.g. for adrenal insufficiency and congenital adrenal hyperplasia.[citation needed]
Medical conditions treated with systemic corticosteroids:[2][4]
- Allergy and respirology medicine
- Asthma (severe exacerbations)
- Chronic obstructive pulmonary disease (COPD)
- Allergic rhinitis
- Atopic dermatitis
- Hives
- Angioedema
- Anaphylaxis
- Food allergies
- Drug allergies
- Nasal polyps
- Hypersensitivity pneumonitis
- Sarcoidosis
- Eosinophilic pneumonia
- Some other types of pneumonia (in addition to the traditional antibiotic treatment protocols)
- Interstitial lung disease
- Dermatology
- Endocrinology (usually at physiologic doses)
- Gastroenterology
- Hematology
- Rheumatology/Immunology
- Ophthalmology
- Other conditions
Topical formulations are also available for the skin, eyes (uveitis), lungs (asthma), nose (rhinitis), and bowels. Corticosteroids are also used supportively to prevent nausea, often in combination with 5-HT3 antagonists (e.g., ondansetron).[citation needed]
Typical undesired effects of glucocorticoids present quite uniformly as drug-induced Cushing's syndrome. Typical mineralocorticoid side-effects are hypertension (abnormally high blood pressure), steroid induced diabetes mellitus, psychosis, poor sleep, hypokalemia (low potassium levels in the blood), hypernatremia (high sodium levels in the blood) without causing peripheral edema, metabolic alkalosis and connective tissue weakness.[5] Wound healing or ulcer formation may be inhibited by the immunosuppressive effects.
A variety of steroid medications, from anti-allergy nasal sprays (Nasonex, Flonase) to topical skin creams, to eye drops (Tobradex), to prednisone have been implicated in the development of central serous retinopathy (CSR).[6][7]
Corticosteroids have been widely used in treating people with traumatic brain injury.[8] A systematic review identified 20 randomised controlled trials and included 12,303 participants, then compared patients who received corticosteroids with patients who received no treatment. The authors recommended people with traumatic head injury should not be routinely treated with corticosteroids.[9]
Pharmacology
Corticosteroids act as agonists of the glucocorticoid receptor and/or the mineralocorticoid receptor.[citation needed]
In addition to their corticosteroid activity, some corticosteroids may have some progestogenic activity and may produce sex-related side effects.[10][11][12][13]
Pharmacogenetics
Asthma
Patients' response to inhaled corticosteroids has some basis in genetic variations. Two genes of interest are CHRH1 (corticotropin-releasing hormone receptor 1) and TBX21 (transcription factor T-bet). Both genes display some degree of polymorphic variation in humans, which may explain how some patients respond better to inhaled corticosteroid therapy than others.[14][15] However, not all asthma patients respond to corticosteroids and large sub groups of asthma patients are corticosteroid resistant.[16]
A study funded by the Patient-Centered Outcomes Research Institute of children and teens with mild persistent asthma found that using the control inhaler as needed worked the same as daily use in improving asthma control, number of asthma flares, how well the lungs work, and quality of life. Children and teens using the inhaler as needed used about one-fourth the amount of corticosteroid medicine as children and teens using it daily.[17][18]
Adverse effects
Summarize
Perspective

Use of corticosteroids has numerous side-effects, some of which may be severe:
- Severe amoebic colitis: Fulminant amoebic colitis is associated with high case fatality and can occur in patients infected with the parasite Entamoeba histolytica after exposure to corticosteroid medications.[19]
- Neuropsychiatric: steroid psychosis,[20] and anxiety,[21] depression. Therapeutic doses may cause a feeling of artificial well-being ("steroid euphoria").[22] The neuropsychiatric effects are partly mediated by sensitization of the body to the actions of adrenaline. Therapeutically, the bulk of corticosteroid dose is given in the morning to mimic the body's diurnal rhythm; if given at night, the feeling of being energized will interfere with sleep. An extensive review is provided by Flores and Gumina.[23]
- Cardiovascular: Corticosteroids can cause sodium retention through a direct action on the kidney, in a manner analogous to the mineralocorticoid aldosterone. This can result in fluid retention and hypertension.
- Metabolic: Corticosteroids cause a movement of body fat to the face and torso, resulting in "moon face", "buffalo hump", and "pot belly" or "beer belly", and cause movement of body fat away from the limbs. This has been termed corticosteroid-induced lipodystrophy. Due to the diversion of amino-acids to glucose, they are considered anti-anabolic, and long term therapy can cause muscle wasting (muscle atrophy).[24] Besides muscle atrophy, steroid myopathy includes muscle pains (myalgias), muscle weakness (typically of the proximal muscles), serum creatine kinase normal, EMG myopathic, and some have type II (fast-twitch/glycolytic) fibre atrophy.[25]
- Endocrine: By increasing the production of glucose from amino-acid breakdown and opposing the action of insulin, corticosteroids can cause hyperglycemia,[26] insulin resistance and diabetes mellitus.[27]
- Skeletal: Steroid-induced osteoporosis may be a side-effect of long-term corticosteroid use.[28][29][30] Use of inhaled corticosteroids among children with asthma may result in decreased height.[31]
- Gastro-intestinal: While cases of colitis have been reported, corticosteroids are often prescribed when the colitis, although due to suppression of the immune response to pathogens, should be considered only after ruling out infection or microbe/fungal overgrowth in the gastrointestinal tract. While the evidence for corticosteroids causing peptic ulceration is relatively poor except for high doses taken for over a month,[32] the majority of doctors as of 2010[update] still believe this is the case, and would consider protective prophylactic measures.[33]
- Eyes: chronic use may predispose to cataract and glaucoma. Clinical and experimental evidence indicates that corticosteroids can cause permanent eye damage by inducing central serous retinopathy (CSR, also known as central serous chorioretinopathy, CSC).[34] This should be borne in mind when treating patients with optic neuritis. There is experimental and clinical evidence that, at least in optic neuritis speed of treatment initiation is important.[35]
- Vulnerability to infection: By suppressing immune reactions (which is one of the main reasons for their use in allergies), steroids may cause infections to flare up, notably candidiasis.[36]
- Pregnancy: Corticosteroids have a low but significant teratogenic effect, causing a few birth defects per 1,000 pregnant women treated. Corticosteroids are therefore contraindicated in pregnancy.[37]
- Habituation: Topical steroid addiction (TSA) or red burning skin has been reported in long-term users of topical steroids (users who applied topical steroids to their skin over a period of weeks, months, or years).[38][39] TSA is characterised by uncontrollable, spreading dermatitis and worsening skin inflammation which requires a stronger topical steroid to get the same result as the first prescription. When topical steroid medication is lost, the skin experiences redness, burning, itching, hot skin, swelling, and/or oozing for a length of time. This is also called 'red skin syndrome' or 'topical steroid withdrawal' (TSW). After the withdrawal period is over the atopic dermatitis can cease or is less severe than it was before.[40]
- In children the short term use of steroids by mouth increases the risk of vomiting, behavioral changes, and sleeping problems.[41]
- Dysphonia: Inhaled corticosteroids are used for treatment of asthma as a standard treatment. This can cause local adverse effects like vocal cord dysfunction.[42]
Biosynthesis

The corticosteroids are synthesized from cholesterol within the adrenal cortex.[1] Most steroidogenic reactions are catalysed by enzymes of the cytochrome P450 family. They are located within the mitochondria and require adrenodoxin as a cofactor (except 21-hydroxylase and 17α-hydroxylase).[citation needed]
Aldosterone and corticosterone share the first part of their biosynthetic pathway. The last part is mediated either by the aldosterone synthase (for aldosterone) or by the 11β-hydroxylase (for corticosterone). These enzymes are nearly identical (they share 11β-hydroxylation and 18-hydroxylation functions), but aldosterone synthase is also able to perform an 18-oxidation. Moreover, aldosterone synthase is found within the zona glomerulosa at the outer edge of the adrenal cortex; 11β-hydroxylase is found in the zona fasciculata and zona glomerulosa.[citation needed]
Classification
Summarize
Perspective
By chemical structure
In general, corticosteroids are grouped into four classes, based on chemical structure. Allergic reactions to one member of a class typically indicate an intolerance of all members of the class. This is known as the "Coopman classification".[43][44]
The highlighted steroids are often used in the screening of allergies to topical steroids.[45]
Group A – Hydrocortisone type
Hydrocortisone, hydrocortisone acetate, cortisone acetate, tixocortol pivalate, prednisolone, methylprednisolone, and prednisone.
Group B – Acetonides (and related substances)
Amcinonide, budesonide, desonide, fluocinolone acetonide, fluocinonide, halcinonide, triamcinolone acetonide, and Deflazacort (O-isopropylidene derivative)
Group C – Betamethasone type
Beclometasone, betamethasone, dexamethasone, fluocortolone, halometasone, and mometasone.
Group D – Esters
Group D1 – Halogenated (less labile)
Alclometasone dipropionate, betamethasone dipropionate, betamethasone valerate, clobetasol propionate, clobetasone butyrate, fluprednidene acetate, and mometasone furoate.
Group D2 – Labile prodrug esters
Ciclesonide, cortisone acetate, hydrocortisone aceponate, hydrocortisone acetate, hydrocortisone buteprate, hydrocortisone butyrate, hydrocortisone valerate, prednicarbate, and tixocortol pivalate.
By route of administration
Topical steroids
For use topically on the skin, eye, and mucous membranes.
Topical corticosteroids are divided in potency classes I to IV in most countries (A to D in Japan). Seven categories are used in the United States to determine the level of potency of any given topical corticosteroid.
Inhaled steroids
For nasal mucosa, sinuses, bronchi, and lungs.[46]
This group includes:
- Flunisolide[47]
- Fluticasone furoate[47]
- Fluticasone propionate[47]
- Triamcinolone acetonide[47]
- Beclomethasone dipropionate[47]
- Budesonide[47]
- Mometasone furoate
- Ciclesonide
There also exist certain combination preparations such as Advair Diskus in the United States, containing fluticasone propionate and salmeterol (a long-acting bronchodilator), and Symbicort, containing budesonide and formoterol fumarate dihydrate (another long-acting bronchodilator).[47] They are both approved for use in children over 12 years old.
Oral forms
Such as prednisone, prednisolone, methylprednisolone, or dexamethasone.[48]
Systemic forms
Available in injectables for intravenous and parenteral routes.[48]
History
Summarize
Perspective
| Corticosteroid | Introduced |
|---|---|
| Cortisone | 1948 |
| Hydrocortisone | 1951 |
| Fludrocortisone acetate | 1954[52] |
| Prednisolone | 1955 |
| Prednisone | 1955[53] |
| Methylprednisolone | 1956 |
| Triamcinolone | 1956 |
| Dexamethasone | 1958 |
| Betamethasone | 1958 |
| Triamcinolone acetonide | 1958 |
| Fluorometholone | 1959 |
| Deflazacort | 1969[54] |
Tadeusz Reichstein, Edward Calvin Kendall, and Philip Showalter Hench were awarded the Nobel Prize for Physiology and Medicine in 1950 for their work on hormones of the adrenal cortex, which culminated in the isolation of cortisone.[55]
Initially hailed as a miracle cure and liberally prescribed during the 1950s, steroid treatment brought about adverse events of such a magnitude that the next major category of anti-inflammatory drugs, the nonsteroidal anti-inflammatory drugs (NSAIDs), was so named in order to demarcate from the opprobrium.[56]
Lewis Sarett of Merck & Co. was the first to synthesize cortisone, using a 36-step process that started with deoxycholic acid, which was extracted from ox bile.[57] The low efficiency of converting deoxycholic acid into cortisone led to a cost of US$200 per gram in 1947. Russell Marker, at Syntex, discovered a much cheaper and more convenient starting material, diosgenin from wild Mexican yams. His conversion of diosgenin into progesterone by a four-step process now known as Marker degradation was an important step in mass production of all steroidal hormones, including cortisone and chemicals used in hormonal contraception.[58]
In 1952, D.H. Peterson and H.C. Murray of Upjohn developed a process that used Rhizopus mold to oxidize progesterone into a compound that was readily converted to cortisone.[59] The ability to cheaply synthesize large quantities of cortisone from the diosgenin in yams resulted in a rapid drop in price to US$6 per gram[when?], falling to $0.46 per gram by 1980. Percy Julian's research also aided progress in the field.[60] The exact nature of cortisone's anti-inflammatory action remained a mystery for years after, however, until the leukocyte adhesion cascade and the role of phospholipase A2 in the production of prostaglandins and leukotrienes was fully understood in the early 1980s.[citation needed]
Corticosteroids were voted Allergen of the Year in 2005 by the American Contact Dermatitis Society.[61]
See also
References
Wikiwand - on
Seamless Wikipedia browsing. On steroids.
