Top Qs
Timeline
Chat
Perspective
Migraine
Disorder resulting in recurrent moderate–severe headaches From Wikipedia, the free encyclopedia
Remove ads
Migraine (UK: /ˈmiːɡreɪn/, US: /ˈmaɪ-/)[1][2] is a complex neurological disorder characterized by episodes of moderate-to-severe headache, most often unilateral and generally associated with nausea, light sensitivity and sound sensitivity.[3][4] Other symptoms may include vomiting, unusual pain, dizziness,[3] and cognitive dysfunction[5]. Some people with migraine experience aura, a period of sensory disturbance at the onset of a migraine attack.[4]
Although primarily considered to be a headache disorder, migraine is highly varied in its clinical presentation and is better thought of as a spectrum disease rather than a distinct clinical entity.[6] Disease burden can range from episodic discrete attacks to chronic disease.[6][7] Incidence of migraines may increase over time, evolving from episodic migraine to chronic migraine. Overuse of acute pain medications may hasten this process and is a risk factor for developing medication overuse headache.[8][9][10]
Migraine is believed to be caused by a combination of genetic, environmental, and neurological factors that influence the behavior of nerve cells, chemical signals and blood vessels within the brain. Migraine attacks are theorized to occur when the brain exceeds an individual sensitivity threshold. Attacks are more likely to occur if stable conditions within the brain are disrupted by changes in hormones, sleep, or stress. The initial phase of a migraine attack starts 48 hours before the main headache phase, with increasing activity in the hypothalamus and the appearance of early (premonitory) symptoms. The subsequent pain phase of a migraine attack may be linked to loss of control between the hypothalamus and the limbic system, and increased activity in the pain pathway from the trigeminal nerve to the brainstem. Release of the neuropeptide CGRP increases blood flow and the transmission of pain signals. Migraineurs display heightened neural sensitivity to stimuli such as light, sound or smell and to pain perception. Mechanisms that normally enable people to habituate to repeated stimuli may be disrupted in migraineurs.[11][12][13]
A migraine management plan often includes lifestyle modifications to cope with migraine triggers and reduce the impact of co-occurring conditions.[14][15][16][17] Non-pharmacological preventive therapies include stress management,[18] improving sleep habits,[19][20][21] eating regularly,[22] and some types of exercise.[23][24][14][15] Initial recommended treatment for acute mild to moderate attacks is with over-the-counter medications such as ibuprofen (Advil, Motrin) and paracetamol (acetaminophen, Tylenol) for pain.[25] Triptans are recommended as a first-line therapy for moderate to severe attacks.[25] The approval of CGRP inhibitors (gepants) is seen as a major advance in migraine treatment.[26][27] According to the American Headache Society, CGRP therapies are a first-line option for migraine prevention.[28][29] Anti-nausea medications are used as a second-line treatment for migraine-related nausea.[25] Ergotamines may be used by those experiencing headaches that do not respond to over-the-counter pain medications.[30][25] Opioids should not be prescribed, because higher doses of opioids are linked to medication overuse headache (MOH) and increased risk of progression from episodic to chronic migraines.[31][32]
Commonly prescribed preventive medications include beta blockers (e.g. metoprolol, propranolol[33]), anticonvulsants (e.g.valproate[33]), antidepressants (e.g. amitriptyline, venlafaxine[33]), calcium channel blockers (e.g. flunarizine[34][35]), and CGRP inhibitors.[35][26][36][37] Medications inhibit migraine through various mechanisms, such as blocking calcium and sodium channels, activation of the neurotransmitter serotonin, and blocking of CGRP transmission in the network of neurons and blood vessels in the brain's protective layers (the meninges).[26]
According to the Global Burden of Disease 2021 database approximately 14% (1.16 billion) of people worldwide are affected by migraine,[38] making it the third most disabling condition affecting the nervous system[39] and one of the most common causes of disability.[40] Beginning at puberty, women experience higher rates than men of incidence, severity of symptoms, and disability related to migraines, in particular to migraine without aura.[41][42][43][44] Occurrence of migraine without aura displays an age-related pattern, beginning around menarche, increasing through the childbearing years, peaking during perimenopause when estrogen levels tend to fluctuate, and tending to decrease following menopause when estrogen levels tend to stabilize.[45] From age 30 to 50, up to 4 times as many women experience migraine attacks as men.[46] Estrogen levels may impact migraine mechanisms of action through blood flow, neurotransmitters, and ion transport across cell membranes.[41][42][43]
Remove ads
Signs and symptoms
Summarize
Perspective
Migraine typically presents as recurrent, mostly unilateral, pulsating headaches, along with heightened reactivity to light, sound, and other sensory stimuli. The severity of the pain, duration of the headache, and frequency of attacks are variable. Symptoms may last for hours or days, seriously affecting quality of life.[47][48]
About 30% of people living with migraine experience episodes with aura.[49][50] Women are more likely than men to experience migraine without aura.[41][42][43][44] Mechanisms in migraine patients with and without aura differ, and it is recommended that these subtypes of migraine be treated separately.[49][50][51]
Migraine attacks can be described in terms of four stages or phases, which may not all be experienced.[47][52] In addition, the period between migraine attacks is sometimes referred to as the interictal phase.[50]
- The premonitory phase or prodrome, generally defined as the 48 hours preceding the pain phase.[47]
- Aura,[47] reversible neurological disturbances (often visual) lasting 5–60 min, generally near onset of the pain phase.[53] These are reported by about 30% of migraineurs.[49][50]
- The pain phase, also known as the headache phase.[47]
- The postdrome, effects following the end of the pain phase of an attack.[47]
A migraine attack lasting longer than 72 hours despite treatment is referred to as status migrainosus. This can lead to complications like dehydration and electrolyte imbalances, and may require emergency room or hospital-level care.[54][55][56]
Migraine is associated with neuropsychiatric disorders including major depression, bipolar disorder, anxiety disorders, obsessive–compulsive disorder, and sleep disorders. Shared neurobiological mechanisms may underly multiple conditions.[57] Co-occurrence with specific psychiatric disorders differs for those experiencing migraine with and without aura.[51]
Prodrome phase
The prodrome phase of migraine is generally defined as the 48 hours preceding the pain or aura phases of an attack.[58] Estimates of the occurrence of premonitory or prodromal symptoms in people with migraine vary widely. Results of a systematic review and metanalysis of studies suggests that around 29% of people with migraine in population-based studies report at least one premonitory symptom, while around 66% of people in clinic populations report premonitory symptoms.[58] These symptoms may include a wide variety of phenomena, including altered mood, irritability, depression or euphoria, fatigue, craving for certain food(s), difficulty speaking or reading, yawning, stiff muscles (especially in the neck), constipation or diarrhea, and sensitivity to smells or noise. Premonitory symptoms may occur with both migraine without aura and migraine with aura.[59][60] Neuroimaging indicates that changes in activity in the limbic system and hypothalamus are associated with prodromal symptoms in migraine.[11][12]
Aura phase
 |  |
 |  |
Aura is a transient neurological event that can occur over 5–60 minutes, generally just prior to the onset of headache pain.[42][61] Symptoms can be visual, sensory or motoric in nature, but visual effects occur most frequently, in as many as 99% of cases of migraine with aura. In rare cases known as persistent aura, aura symptom may remain after 60 minutes.[62]
Visual disturbances often consist of a scintillating scotoma (an area of partial alteration in the field of vision, which flickers and may interfere with a person's ability to read or drive). These typically start near the center of vision and then spread out to the sides with zigzagging lines, which have been described as looking like fortifications or walls of a castle. Usually, the lines are in black and white, but some people also see colored lines. Some people lose part of their field of vision known as hemianopsia while others experience blurring.[63][64][65]
Sensory auras are the second most common type; they occur in 30–40% of people with auras. Often, a feeling of pins-and-needles begins on one side in the hand and arm and spreads to the nose–mouth area on the same side. Numbness usually occurs after the tingling has passed with a loss of position sense. Other symptoms of the aura phase can include speech or language disturbances, world spinning, and, less commonly, motor problems. Motor symptoms indicate that this is a hemiplegic migraine, and weakness often lasts longer than one hour unlike other auras.[66]
Pain phase
Classically the headache is unilateral, throbbing, and moderate to severe in intensity.[47] The feeling of pulsating pain is not in phase with the pulse.[67] In around 40% of cases, the pain may be bilateral, affecting both sides of the head.[68] The pain usually lasts 4 to 72 hours in adults.[68] Pediatric and adolescent migraines differ from adult presentations, more often involving bilateral headaches with shorter duration.[69]
Pain is frequently accompanied by nausea, vomiting, sensitivity to light, sensitivity to sound, sensitivity to smells, fatigue, and irritability. Many prefer a dark and quiet environment, and seek to avoid stimuli to which they are sensitive. Nausea occurs in almost 90% of people, and vomiting occurs in about one-third.[55][36][70] Other symptoms may include blurred vision,[65] sino-nasal symptoms such as nasal stuffiness,[71] diarrhea,[72] neck pain,[73] and swelling or tenderness of the scalp.[74] In rare cases of migraine with brainstem aura (basilar migraine), neurological symptoms related to the brain stem may affect both sides of the body, including a sense of the world spinning, light-headedness, and confusion.[75]
During the pain phase, motion and physical activity may increase pain. Migraineurs are likely to decrease physical activity during this time.[76] However, the effects of physical activity on migraine are complex, and regular exercise on an on-going basis may have a preventive effect and decrease frequency of migraine attacks.[23][77]
Silent migraine
It has been suggested that aura may occur without a subsequent headache.[78] This is referred to in modern classification as a typical aura without headache, or acephalgic migraine in previous classification, or commonly as a "silent migraine".[79][80] Symptoms such as visual disturbance, vision loss, alterations in color perception, and sensitivity to light, sound, and odors may still be debilitating in the absence of pain.[47]
Postdrome
The migraine postdrome, sometimes referred to as the "migraine hangover", is the constellation of symptoms occurring after the acute headache has ceased. ICHD-3 defines this as the 48 hours after the pain ceases. Common symptoms include tiredness, difficulty concentrating, mood changes, and thirst.[81] Other symptoms reported include dizziness and euphoria.[3]
Remove ads
Causes
Summarize
Perspective
Migraine is believed to result from a mix of genetic, environmental, and neurological factors.[11] Migraine runs in families, with heritability estimates of 34–64%, but this rarely reflects a single gene defect. Rather, a variety of genetic factors may relate to neuronal, vascular and other systems, and create genetic susceptibility.[82] Migraine often occurs with conditions such as depression, anxiety, and bipolar disorder, which may have a bidirectional relationship (either one can worsen the other). It is likely that shared genetic and neurobiological mechanisms contribute to risk factors that underlie multiple conditions.[83][84]

Genetics
Studies of twin adults indicate a 0.36 to 0.48 genetic influence on the likelihood of developing migraine. However, few studies examine non-European populations, or distinguish between migraine with aura and migraine without aura.[85] It is clear from family and populations studies that migraine is a complex disorder, where numerous genetic risk variants exist, and where each variant increases the risk of migraine marginally.[86][87] It is also known that having several of these risk variants increases the risk by a small to moderate amount.[82]
Single gene disorders that result in migraine are rare. One of these is known as familial hemiplegic migraine, a type of migraine with aura, which is inherited in an autosomal dominant fashion. Three main genes have been shown to be involved in familial hemiplegic migraine via ion transport: CACNA1A, ATP1A2, and SCN1A (FHM3). The axonal protein PRRT2, associated with the exocytosis complex, may be a fourth causal gene for FHM, but this is still under debate.[82]
Another genetic disorder that has been associated with migraine is CADASIL syndrome or cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Despite some similarities in symptoms, ICHD-3 recommends that this be diagnosed "headache attributed to CADASIL" (code 6.8.1) rather than migraine with aura (MA) or migraine without aura (MO) (codes 1.1 and 1.2).[88] The TRPM8 gene, which codes for a cation channel, has been linked to migraine.[89][90] One meta-analysis found a protective effect from angiotensin converting enzyme polymorphisms on migraine.[91][33]
The common forms of migraine are polygenetic, where common variants of numerous genes contribute to the predisposition for migraine.[82] These genes can be placed in three categories: increasing the risk of migraine in general, specifically migraine with aura, or migraine without aura.[92][93] Three of these genes, CALCA, CALCB, and HTR1F are already target for migraine specific treatments. Five genes are specific risk to migraine with aura, PALMD, ABO, LRRK2, CACNA1A and PRRT2, and 13 genes are specific to migraine without aura. Using the accumulated genetic risk of the common variations, into a so-called polygenetic risk, it is possible to assess e.g. the treatment response to triptans.[94][95]
Triggers
A migraine trigger reduces the threshold at which a migraine attack occurs in someone who is predisposed to migraine.[96][59][26][97] Categories of hypothesized migraine triggers include emotion, nutrition, sleep disturbance, hormones, weather, sensory overstimulation and strenuous exercise.[98] Migraine triggers may be classified as internal, modifying the body's homeostasis (e.g. hormonal variability, stress, sleep disturbance, fasting) or external, originating outside the body and influencing the perception of sensory signals (e.g. temperature fluctuations, noises, and odors). In some cases, factors reported as triggers (e.g. sensory sensitivities, food cravings and mood change) may be more appropriately considered as premonitory symptoms resulting from changes in brain activity during the prodromal phase of migraine.[59][26][96][97] Determining whether and when something acts as a true causal trigger, and when it is a symptom of already-occurring changes, is an ongoing area of study.[59]
Studies of the brain's structure and function indicate that brain activity changes during the 48 (or even 72) hours before the pain phase of migraine. During this initial phase of a migraine attack, people may report prodromal/premonitory symptoms (PSs) such as fatigue, yawning, difficulty concentrating, mood changes, dizziness, neck pain, light sensitivity, food cravings, and nausea. Such symptoms may continue into the pain phase and postdrome.[59] Some studies suggest that PSs may be linked to activity in particular neuroanatomical pathways and areas of the brain. Yawning, food cravings, homeostatic regulation, and sleep disturbance may be linked to activation in the hypothalamus. Other PSs, such as neck pain and nausea, may be related to activity in the brainstem.[59] The stimuli that are found disturbing vary from person to person.[99] Those experiencing PSs can sometimes correctly predict an oncoming attack.[59]
The extent to which a possible trigger has an actual causal connection with headache onset is uncertain in most cases, and some relationships may be bidirectional.[83][84] However, there are strong associations between migraine and hormonal changes, stress, quality of sleep, and fasting. It has been theorized that these "catalyst triggers" may act by increasing activity in the hypothalamus or trigeminal system and exceeding the brain's migraine threshold.[59] Lifestyle changes that help to maintain bodily homeostasis, such as regular sleep, managing of stress, and eating regularly, can be helpful interventions.[100] Whether a possible trigger is a cause or an early symptom of a migraine attack, it may help to manage exposure to sensory stimuli such as smells, lights, sound or touch.[99]
Hormonal changes
From puberty onwards, women experience migraine attacks at greater rates and with greater severity of symptoms than men.[42] Women are more likely than men to experience migraine without aura. A population-based study in Denmark suggests that sex differences in rate and severity of migraine attacks almost exclusively reflect the incidence of migraine without aura (11% in females and 3.59% in males). In comparison, sex differences were not significant in migraine with aura (1.72% in females and 1.58% in males).[44]
Patterns of migraine attacks in men and women begin to diverge at the onset of puberty, as a result of changes in sex hormones.[42] The incidence of attacks of migraine without aura is strongly related to hormonal fluctuations in estrogen, which varies monthly and across a woman's lifespan.[101] Migraine episodes are more likely to occur immediately before and during menstruation, possibly due to the drop in estrogen levels prior to the menstrual period.[102]
Occurrence of migraine without aura displays an age-related pattern.[42][41] First onset of migraine is often reported around menarche, and prevalence increases from early adulthood throughout the childbearing years.[44] Incidence and severity of migraine without aura peaks between ages 35 and 50.[41][45] Attacks may worsen during perimenopause due to irregular periods and fluctuating estrogen levels. The first onset of migraine may occur during perimenopause.[46][45] Following menopause, estrogen levels tend to stabilize at a lower rate, and migraine frequency and severity are likely to decrease.[42][45]
Hormonal changes may also affect incidence and occurrence of migraines in relation to pregnancy.[103] Migraine episodes tend to diminish during the 2nd and 3rd trimesters of pregnancy, when elevated estrogen levels are stable. They are likely to return following the abrupt drop in estrogen levels after childbirth.[42]
Relationships between oral contraceptive use and migraine are less clear, and may differ depending on migraine type, age, and characteristics of the menstrual cycle. In some cases, use of oral contraceptives or hormone replacement therapy can help to stabilize estrogen levels and prevent migraines,[102] while suddenly ceasing to use hormonal contraceptives may be associated with increased attacks.[42]
Women who experience migraine with aura differ from women who experience migraine without aura in onset, symptoms and recommended treatments. Women who perceive aura are more likely to have experienced the first onset of migraine before menarche.[45] For women who experience migraine with aura, migraines are less likely to improve during pregnancy, and use of oral contraceptives is more likely to worsen attacks. Women with migraine with aura who use combined hormonal contraceptives (ethinylestradiol dose between 20 and 40 μg) have a higher risk of ischemic stroke.[42]
Stress
The headache trigger that people are most aware of is stress, ranking first in reports for men, and second to hormonal factors for women.[96][18] Best practices for psychologically addressing stress as a possible migraine trigger include relaxation therapy, biofeedback, and cognitive behavioral therapy (CBT).[104] Activities such as relaxation therapy are more likely to be effective when used as a routine part of daily life or to address incidents of stress as a risk factor, rather than during the pain phase of a migraine attack.[105]
Sleep
Migraineurs report a variety of sleep-related issues as possible triggers. These include undersleeping, irregular sleep, frequent night-time waking, and oversleeping. Those who experience chronic migraine may be less likely to maintain consistent sleep habits than those who experience episodic migraines.[15] Jet-lag, shift work, and other disruptions of circadian rhythms may increase migraines.[106][107][108] Changes in migraine frequency have been reported in relation to changes between daylight savings time and standard time.[109]
Sleep habits have been shown to be negatively affected by factors such as air quality and exposure to ambient and indoor pollutants.[110] A nationwide study of household fuel use in China found that those using solid fuel rather than clean fuel were more likely to develop migraines; those who switched from solid fuels to clean fuels showed a lower risk of migraines. However, those who used solid fuel but reported good sleep duration were not at a significantly higher risk for migraines, suggesting that sleep played a protective role.[111] Sleep hygiene improvements and maintaining a consistent sleep schedule are among the most frequently recommended migraine management techniques.[112] [19][20][21]
Diet
Fasting or missed meals are a commonly perceived trigger for migraines, and dietary modifications are a frequent management technique.[15] Missing meals like breakfast can reduce brain glucose levels, leading to hypoglycemia and triggering the release of stress hormones like cortisol and adrenaline, which can affect migraines. Irregular meals are particularly strong predictors of attacks for those experiencing chronic migraines. Eating balanced meals at consistent times and hydrating well can help to prevent migraines and lessen migraine symptoms.[113]
A wide variety of specific foods and drinks have been reported as possible triggers, including alcohol, coffee, chocolate, cheese, nuts, citrus fruits, fatty foods, processed meats, monosodium glutamate, and aspartame.[113] Mechanisms of action have been proposed for some of the commonly reported foods and drinks, such as red and white wine, hot dogs, and chocolate.[96] Tyramine, which is naturally present in alcoholic beverages, most cheeses, processed meats, and other foods may trigger migraine symptoms in some individuals.[114][115] Tyramine is also present at low levels in chocolate.[116] Monosodium glutamate (MSG) has been reported as a trigger for migraine in some individuals, but whether or not there is a causative relationship continues to be debated.[117]
People may experience food cravings as a result of changes in brain activity during the prodromal phase of migraine. Reports that foods such as chocolate are triggers may actually reflect a increased desire for such foods as an early symptom of migraine attacks.[118][59]
Sensory sensitivity
Sensitivity to light (photophobia), sensitivity to sound (phonophobia), and sensitivity to smells (osmophobia) are often reported as migraine triggers. Some migraineurs may also report sensitivity to touch (allodynia).[36][70] Neuroimaging and neurophysiological studies show changes in sensory thresholds relating to sensitivity to light, sound and smell and to pain perception.[59][119] Patient reports of sensitivity triggers may be early symptoms in the premonitory phase of a migraine attack.[120] People often deal with migraine attacks by seeking a dark and quiet space, and avoiding further sensory stimulation including movement, light, sounds, touch or smells.[70]
Light
Sensitivity to light is a common symptom in migraine. Discomfort is associated with four categories of stimulation: bright light, flickering light, pattern, and color. While retinal mechanisms also may be involved, cortical mechanisms are increasingly seen as explaining discomfort from all four types of visual stimulation.[121]
People have been shown to have different thresholds for discomfort from stimuli. During migraine, stimulation can provoke a hyper-excitable cortical response involving specific subsets of neurons. Thresholds at which a response occurs and the size of the response that occurs may both be involved. For example, those with a more sensitive discomfort glare threshold have been shown to display greater activity in the cunei, lingual gyri and superior parietal lobules in response to peripheral lights. Photophobia may reflect individual differences in homeostatic response to stimuli, in which cortical hyper-excitability is further aggravated by visual stimulation.[121] Those who are less sensitive to light may better reduce discomfort and avoid over-stimulation.[122][121] It has been suggested that migraineurs may experience dysfunction in inhibitory mechanisms, have difficulty habituating to ongoing stimuli, and even become sensitized to such stimuli.[123]
Strategies for reducing discomfort may include staying in a darkened room, wearing sunglasses or hats to avoid direct sunlight and minimize glare, using fluorescent light filters to soften and diffuse light and reduce flicker,[14] using green lights in preference to other colors,[124] and using anti-glare filters with computers. Evaluating the ergonomics of workspaces and using suitable chairs and proper posture while working, may also be helpful.[14]
Sound
Migraineurs frequently report hypersensitivity to auditory stimuli. Research indicates that they may have lower hearing thresholds[125] and lower thresholds of discomfort for sounds than non-migraineurs generally, not just during migraine attacks.[126] Migraineurs also have lower hearing thresholds than usual while they are experiencing headaches. Lower hearing threshold correlates with headache frequency, and with frequency of auditory, visual, and tactile triggers. Phonophobia in migraineurs correlates with higher brainstem neuronal excitability.[125][127] There is some evidence suggesting that migraineurs experience an increase or potentiation in response to blocks of sound, rather than habituation.[70]
Smell
Osmophobia is a possible diagnostic marker of migraine, distinguishing it from other types of headaches.[128] Migraineurs may report increased aversion to a smell that would not be unpleasant normally, heightened awareness of a smell, or other olfaction-related symptoms.[129][99] Osmophobia is more often observed in people with a longer history of migraines and greater migraine-related impairment. This may suggest that sensitivity to stimuli increases over time.[130] Migraineurs who experience scent-related symptoms are more likely to experience insomnia, depression, fatigue and neuropathic pain, and to report lower quality of life than those without osmophobia.[131]
The brain processes odorous stimuli through the olfactory, trigeminal, and pheromone systems. There is evidence that different odors may activate different brain regions. Reported trigger smells have been grouped into six general categories of products: oil derivatives and others; fetid odor; cooking; shampoos and conditioners; cleaning products; and perfumes, insecticides, and rose.[120] Perfumes were the smells most frequently reported in connection with migraine attacks.[120][132][133] There is evidence that those with chronic migraines are more likely than those with episodic migraines to be sensitive to floral scents in various types of products. Strategies for reducing scent exposure include using fragrance-free products, improving ventilation and air quality, wearing masks, and using air cleaners.[120][99]
Weather
Migraines have been reported to be triggered by changes in weather conditions such as temperature, ambient pressure, and humidity, but studies have shown mixed results.[134][135][136][96]
Remove ads
Mechanism
Summarize
Perspective
Migraine is a complex neurovascular pain disorder involving blood vessels, neurons, and cerebrospinal fluid within the meninges, the brain's protective layers. The areas involved are sometimes referred to as the trigeminovascular system. The trigeminal nerve, located within the dura mater, carries sensory information about pain, touch, heat and cold from the face to the brain. The hypothalamus receives input from the trigeminal nerve and can modulate trigeminal nerve activity.[137][138][139] Migraine patients appear to experience impairments in cortical habituation, a process which would normally decrease cortical responses to repetitive sensory stimuli.[140][141]
Initiation of a migraine attack may begin with disruption in the hypothalamus and limbic system.[137][138][139] Gradually increasing hypothalamic activity has been observed in the period leading up to a migraine attack, followed by a disruption or collapse of hypothalamic connectivity to the limbic system during an attack.[142] Disruption of the connection between the hypothalamus and limbic system may increase activity in the pain pathway from the trigeminal nerve to the brain, resulting in a migraine attack.[137][138][139]
The meninges, particularly the dura mater, are rich in pain-sensitive nerve endings. Sensory information travels along trigeminal nerve fibers to cell bodies located within the trigeminal ganglion (TG). Axons of the trigeminal ganglion neurons enter the brainstem and travel to the trigeminal nucleus caudalis (TNC).[143][139][144]
The activity of calcitonin gene-related peptide (CGRP) in the meninges is linked to migraine.[12] CGRP is released from both the trigeminal ganglion (TG) and the trigeminal nucleus caudalis (TNC) in response to trigeminal nerve activation. CGRP activates receptors on meningeal blood vessels, causing dilation and changes in blood flow. CGRP also activates specialized nerve endings in the dura mater (nociceptors) that transmit pain signals to the central nervous system. Increased neuronal activity in the trigeminal pain pathway reaches higher cortical pain regions via the brainstem, midbrain, and thalamus.[137][139]
Stimulation of the trigeminal nerve may result in release of neuropeptides such as CGRP, vasodilation of cerebral and dural blood vessels, neurogenic inflammation, and the transmission of pain signals via nerves in the meninges.[12] Cerebrospinal fluid may also play a role in migraine by conveying signals from the brain to overlying pain-sensitive meningeal tissues, including the dura mater.[12]
The experience of aura in migraine is associated with cortical spreading depression (CSD) at the onset of a migraine attack. In cortical spreading depression, a wave of depolarization propagates across the cerebral cortex, followed by suppression of spontaneous neuronal activity. Physiologically, CSD involves an influx of sodium and calcium ions in concentrations that overwhelm the cell membrane's transport capability. Dysregulation of electrolyte concentration and disruption of homeostasis then spread to other cortical regions.[145][146]
Incidence of migraines may increase over time, evolving from episodic migraine to chronic migraine. Overuse of acute pain medications may hasten this process of chronification, and is a risk factor in developing medication overuse headache.[8][9][10]
Remove ads
Diagnosis
Summarize
Perspective
The diagnosis of a migraine is based on signs and symptoms.[48] A headache calendar is a useful diagnostic tool for tracking the date, duration, and symptoms of headaches. Migraine can be classified according to whether the patient experiences an aura (MA) or not (MO) and frequency of headaches (episodic or chronic).[36] According to the International Classification of Headache Disorders (ICHD-3), migraine diagnosis is primarily clinical and is based on identifying characteristic patterns of headache features and associated symptoms rather than laboratory or imaging findings [147]Neuroimaging tests are not necessary to diagnose migraine, but may be used to find other causes of headaches in those whose examination and history do not confirm a migraine diagnosis.[148] The American Headache Society's evidence-based guideline recommends neuroimaging only when "red-flag" symptoms or abnormal neurological findings are present, noting that routine imaging is unnecessary for patients who already meet clinical criteria for migraine.[149] </references>It is believed that a substantial number of people with the condition remain undiagnosed.[48]
The diagnosis of migraine without aura, according to the International Headache Society, can be made according to the "5, 4, 3, 2, 1 criteria", which is as follows:[52]
- Five or more attacks – for migraine with aura, two attacks are sufficient for diagnosis.
- Four hours to three days in duration
- Two or more of the following:
- Unilateral (affecting one side of the head)
- Pulsating
- Moderate or severe pain intensity
- Worsened by or causing avoidance of routine physical activity
- One or more of the following:
- Nausea and/or vomiting
- Sensitivity to both light (photophobia) and sound (phonophobia)
If someone experiences two of the following: photophobia, nausea, or inability to work or study for a day, the diagnosis is more likely.[150] In those with four out of five of the following: pulsating headache, duration of 4–72 hours, pain on one side of the head, nausea, or symptoms that interfere with the person's life, the probability that this is a migraine attack is 92%.[151] In those with fewer than three of these symptoms, the probability is 17%.[151]
Classification
Migraine was first comprehensively classified in 1988, when the International Headache Society (IHS) began its classification of headache disorders.[152] The IHS updated its classification of headaches in 2004.[52] A third version was published in 2018.[153] According to this classification, migraine is a primary headache disorder along with tension-type headaches and cluster headaches.[154]
Migraine is divided into six subclasses (some of which include further subdivisions):[155]
- Migraine without aura, or "common migraine", involves migraine headaches that are not accompanied by aura.
- Migraine with aura, or "classic migraine", usually involves migraine headaches accompanied by aura. Less commonly, aura can occur without a headache or with a nonmigraine headache.
- Subtype of migraine with aura: hemiplegic migraine and sporadic hemiplegic migraine, in which a person has migraine with aura and with accompanying motor weakness. If a close relative has had the same condition, it is called "familial"; otherwise, it is called "sporadic".
- Subtype of migraine with aura: basilar-type migraine, where a headache and aura are accompanied by difficulty speaking, world spinning, ringing in ears, or several other brainstem-related symptoms, but not motor weakness. This type was initially believed to be due to spasms of the basilar artery, the artery that supplies the brainstem. Now that this mechanism is not believed to be primary, the symptomatic term migraine with brainstem aura (MBA) is preferred.[75] Retinal migraine (which is distinct from visual or optical migraine) involves migraine headaches accompanied by visual disturbances or even temporary blindness in one eye.
- Childhood periodic syndromes that are commonly precursors of migraine include cyclical vomiting (occasional intense periods of vomiting), abdominal migraine (abdominal pain, usually accompanied by nausea), and benign paroxysmal vertigo of childhood (occasional attacks of vertigo).
- Complications of migraine describe migraine headaches and/or auras that are unusually long or unusually frequent, or associated with a seizure or brain lesion.
- Probable migraine describes conditions that have some characteristics of migraine, but where there is not enough evidence to diagnose it as migraine with certainty (in the presence of concurrent medication overuse).
- Chronic migraine is a complication of migraine, and is a headache that fulfills diagnostic criteria for migraine headache and occurs for a greater time interval. Specifically, greater than or equal to 15 days/month for longer than 3 months.[156]
Abdominal migraine
Abdominal migraine is most frequently diagnosed in children, but occasionally in adults. Diagnostic criteria for abdominal migraine are outlined by both the Rome IV and ICHD III classification systems. Criteria include repeated, acute, paroxysmal attacks of abdominal pain that may be associated with nausea and vomiting. Attacks last for at least 1 hour and interfere with normal life. Average attack duration has been reported as 17 hours. Abdominal migraine often occurs in people with either a personal or family history of typical migraine, and children may develop typical migraine later in life. Abdominal migraine, migraine, and cyclical vomiting syndrome share common symptoms.[157]
Differential diagnosis
Other conditions that can cause similar symptoms to a migraine headache include temporal arteritis, cluster headaches, acute glaucoma, meningitis and subarachnoid hemorrhage.[151] Temporal arteritis typically occurs in people over 50 years old and presents with tenderness over the temple. Cluster headache presents with one-sided nose stuffiness, tears and severe pain around the orbits. Acute glaucoma is associated with vision problems. Meningitis associated with fever. Subarachnoid hemorrhage is associated with a very fast onset.[151] Tension headaches typically occur on both sides, are not pounding, and are less disabling.[151]
Those with stable headaches that meet criteria for migraine should not receive neuroimaging to look for other intracranial disease.[148]
Remove ads
Management
Summarize
Perspective
Management of migraine includes both prevention of migraine attacks and acute treatment. Preventive (prophylactic) treatment can be given in the absence of a headache to reduce the frequency and severity of future attacks. Acute (abortive) treatment attempts to diminish or reverse the progression of a headache that has already started. Measures for reducing and avoiding triggers may also be beneficial.[158] Headache tracking, using a headache diary or smartphone app, is a standard self-management tool used to monitor migraineurs' frequency of headache occurrence, associated symptoms or triggers, and effects of treatments.[159]
A migraine management plan often includes lifestyle modifications to cope with migraine triggers and reduce the impact of comorbidities.[14][15][16] Recommended lifestyle modifications promote maintaining a consistent lifestyle, through regular sleep patterns,[19][20][21] regular eating, staying hydrated,[22] managing stress,[18] engaging in moderate exercise, and maintaining a healthy body weight.[24][14][15] Avoiding dietary triggers and caffeine overuse may also be recommended lifestyle modifications.[100] Data suggests that sleep modification may be particularly helpful in reducing migraine frequency for adults with chronic migraines.[160]
Behavioral techniques that have been utilized in the treatment of migraines include Cognitive Behavioral Therapy (CBT), relaxation training, biofeedback, Acceptance and Commitment Therapy (ACT), as well as mindfulness-based therapies.[160] A 2024 systematic literature review and meta analysis found evidence that treatments such as CBT, relaxation training, ACT, and mindfulness-based therapies can reduce migraine frequency both on their own and in combination with other treatment options.[160] In addition, it was found that relaxation therapy aided in the lessening of migraine frequency when compared to education by itself.[160] Similarly, for children and adolescents, CBT and biofeedback strategies are effective in decreasing of frequency and intensity of migraines. These techniques often include relaxation methods and promotion of long-term management without medication side effects, which is emphasized for younger individuals.[160]
A variety of possible diets have been proposed, including ketogenic diet,[161][162] Mediterranean diet, DASH diet, and high intakes of fruits, vegetables, legumes, and oil seeds.[163] Further research is needed to examine whether and when dietary interventions are beneficial to migraineurs.[22] Interventions such as transcranial magnetic stimulation and transcutaneous supraorbital nerve stimulation require further research.[164][165]
Acute treatments are most effective when administered early in an attack.[166] Initial recommended treatment for acute mild to moderate attacks is with over-the-counter (OTC) medications such as ibuprofen (Advil, Motrin) and paracetamol (acetaminophen, Tylenol) for pain.[25] Triptans are recommended as a first-line therapy for moderate to severe attacks.[25] The approval of CGRP inhibitors (gepants) is seen as a major advance in migraine treatment.[26][27] According to the American Headache Society, CGRP targeting therapies are a first-line option for migraine prevention.[28][29] Anti-nausea medications are used as a second-line treatment for migraine-related nausea.[25] Ergotamines may be used by those experiencing headaches that do not respond to over-the-counter pain medications.[30][25] Opioids should not be prescribed, as higher doses of opioids are linked to medication overuse headache (MOH) and increased risk of progression from episodic to chronic migraines.[31][32]
Systematic review and network meta analysis comparing the effectiveness of medications for acute migraine attacks in adults suggest that triptans, ditans, and gepants are all associated with reduced pain after 2 hours, with triptans being the most successful in reducing pain. Gepants were the least likely to involve adverse events, with some triptans having a higher risk than gepants, and ditans having the highest risk among all treatments.[167]
Preventive medications may be recommended for those experiencing frequent or severe migraines.[166] Preventive medications include beta blockers, topiramate, and calcitonin gene related peptides (CGRP) inhibitors like erenumab and galcanezumab, which have demonstrated significant efficacy in clinical studies.[168] Prokinetic antiemetics are used as adjunctives for patients with nausea and/or vomiting.[68] Corticosteroids such as dexamethasone have been used to treat patients with status migrainosus,[169] severe baseline disability, or refractory or recurrent headaches.[170][171]
Remove ads
Prognosis
Summarize
Perspective
"Migraine exists on a continuum of different attack frequencies and associated levels of disability."[172] For those with occasional, episodic migraine, a "proper combination of drugs for prevention and treatment of migraine attacks" can limit the disease's impact on patients' personal and professional lives.[173] Fewer than half of people with migraine seek medical care.[174] Severe migraine ranks in the highest category of disability, according to the World Health Organization, which uses metrics to determine disability burden,[175] and the bulk of disability burden is due to chronic (as opposed to episodic) migraine.[176]
Repeated experiences of pain, including migraine pain, cause functional and structural changes in the brain[176] It is possible for migraine to progress from an occasional inconvenience to a life-changing, chronic disorder. This "chronification" affects 3% of migraineurs in a given year, such that 8% of migraineurs have chronic migraine in any given year. Brain imagery reveals that the electrophysiological changes seen during an attack become permanent in people with chronic migraine; "thus, from an electrophysiological point of view, chronic migraine indeed resembles a never-ending migraine attack."[176]
Factors such as genetic predisposition and hormones complicate the risk profile of those with migraine. There are significant differences between women who do and do not experience aura in terms of symptoms, mechanisms, and treatment.[42][177] Migraine with aura is associated with an increased risk of ischemic stroke, myocardial infarction, coronary artery disease, and coronary artery dissection (SCAD). This may reflect shared underlying mechanisms of migraine with aura and cardiovascular disease.[177] Women who experience migraine with aura and use estrogen-containing oral contraceptives have a higher risk of ischemic stroke.[42][177] In contrast, migraine generally, and migraine without aura, do not appear be related to increased risk of stroke or heart disease.[178] Preventative therapy, particularly for those with migraine with aura, may prevent associated strokes.[179]
People with migraine, particularly women, may develop higher than average numbers of white matter brain lesions of unclear significance.[5]
Remove ads
Epidemiology
Summarize
Perspective

Migraine is common, with around 33% of women and 18% of men affected at some point in their lifetime.[46] Onset can be at any age, but prevalence rises sharply around puberty, and remains high until declining after age 50.[46] Before puberty, boys and girls are equally impacted, with around 5% of children experiencing migraine attacks. From puberty onwards, women experience migraine attacks at greater rates than men. From age 30 to 50, up to 4 times as many women experience migraine attacks as men;[46] this is most pronounced in migraine without aura.[44]
According to the Global Burden of Disease 2021 database approximately 14% (1.16 billion) of people worldwide are affected by migraine.[38] In the United States, about 6% of men and 18% of women experience a migraine attack in a given year, with a lifetime risk of about 18% and 43%, respectively.[48] In Europe, migraine affects 12–28% of people at some point in their lives, with about 6–15% of adult men and 14–35% of adult women getting at least one attack yearly.[180] Rates of migraine are slightly lower in Asia and Africa than in Western countries.[181] Chronic migraine occurs in approximately 1.4–2.2% of the population.[182]
Remove ads
Economic impact
Migraine is a significant source of both medical costs and lost productivity. It has been estimated that migraine is the most costly neurological disorder in the European Community, costing more than €27 billion per year.[183] In the United States, direct costs have been estimated at US$17 billion, while indirect costs – such as missed or decreased ability to work – is estimated at US$15 billion.[184] Nearly a tenth of the direct cost is due to the cost of triptans.[184] In those who do attend work during a migraine attack, effectiveness is decreased by around a third.[183] Negative effects also frequently occur for a person's family.[183]
Remove ads
History
Summarize
Perspective
An early description consistent with migraine is contained in the Ebers Papyrus, written around 1500 BCE in ancient Egypt.[185]
The word migraine is from the Greek ἡμικρᾱνίᾱ (hēmikrāníā), 'pain in half of the head',[186] from ἡμι- (hēmi-), 'half' and κρᾱνίον (krāníon), 'skull'.[187]
In 200 BCE, writings from the Hippocratic school of medicine described the visual aura that can precede the headache and a partial relief occurring through vomiting.[188]
A second-century description by Aretaeus of Cappadocia divided headaches into three types: cephalalgia, cephalea, and heterocrania.[189] Galen of Pergamon used the term hemicrania (half-head), from which the word migraine was eventually derived.[189] Galen also proposed that the pain arose from the meninges and blood vessels of the head.[188] Migraine was first divided into the two now used types – migraine with aura (migraine ophthalmique) and migraine without aura (migraine vulgaire) in 1887 by Louis Hyacinthe Thomas, a French librarian.[188] The mystical visions of Hildegard von Bingen, which she described as "reflections of the living light", are consistent with the visual aura experienced during migraine attacks.[190]

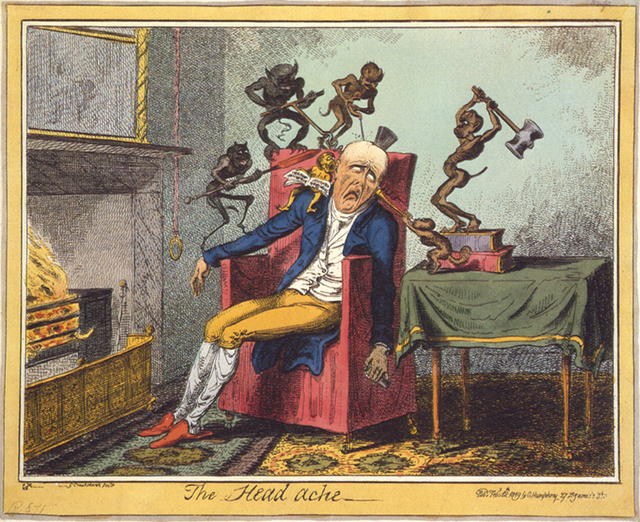
Trepanation, the deliberate drilling of holes into a skull, was practiced as early as 7,000 BCE.[185] While sometimes people survived, many would have died from the procedure due to infection.[191] It was believed to work via "letting evil spirits escape".[192] William Harvey recommended trepanation as a treatment for migraine in the 17th century.[193] The association between trepanation and headaches in ancient history may simply be a myth or unfounded speculation that originated several centuries later. In 1913, the world-famous American physician William Osler misinterpreted the French anthropologist and physician Paul Broca's words about a set of children's skulls from the Neolithic age that he found during the 1870s. These skulls presented no evident signs of fractures that could justify this complex surgery for mere medical reasons. Trepanation was probably born of superstitions, to remove "confined demons" inside the head, or to create healing or fortune talismans with the bone fragments removed from the skulls of the patients. However, Osler wanted to make Broca's theory more palatable to his modern audiences, and explained that trepanation procedures were used for mild conditions such as "infantile convulsions headache and various cerebral diseases believed to be caused by confined demons."[194]
While many treatments for migraine have been attempted, it was not until 1868 that use of a substance that eventually turned out to be effective began.[188] This substance was the fungus ergot from which ergotamine was isolated in 1918[195] and first used to treat migraine in 1925.[196] Methysergide was developed in 1959 and the first triptan, sumatriptan, was developed in 1988.[195] During the 20th century, with better study design, effective preventive measures were found and confirmed.[188]
Remove ads
See also
References
Further reading
External links
Wikiwand - on
Seamless Wikipedia browsing. On steroids.
Remove ads

