Top Qs
Timeline
Chat
Perspective
Calcifediol
Chemical compound From Wikipedia, the free encyclopedia
Remove ads
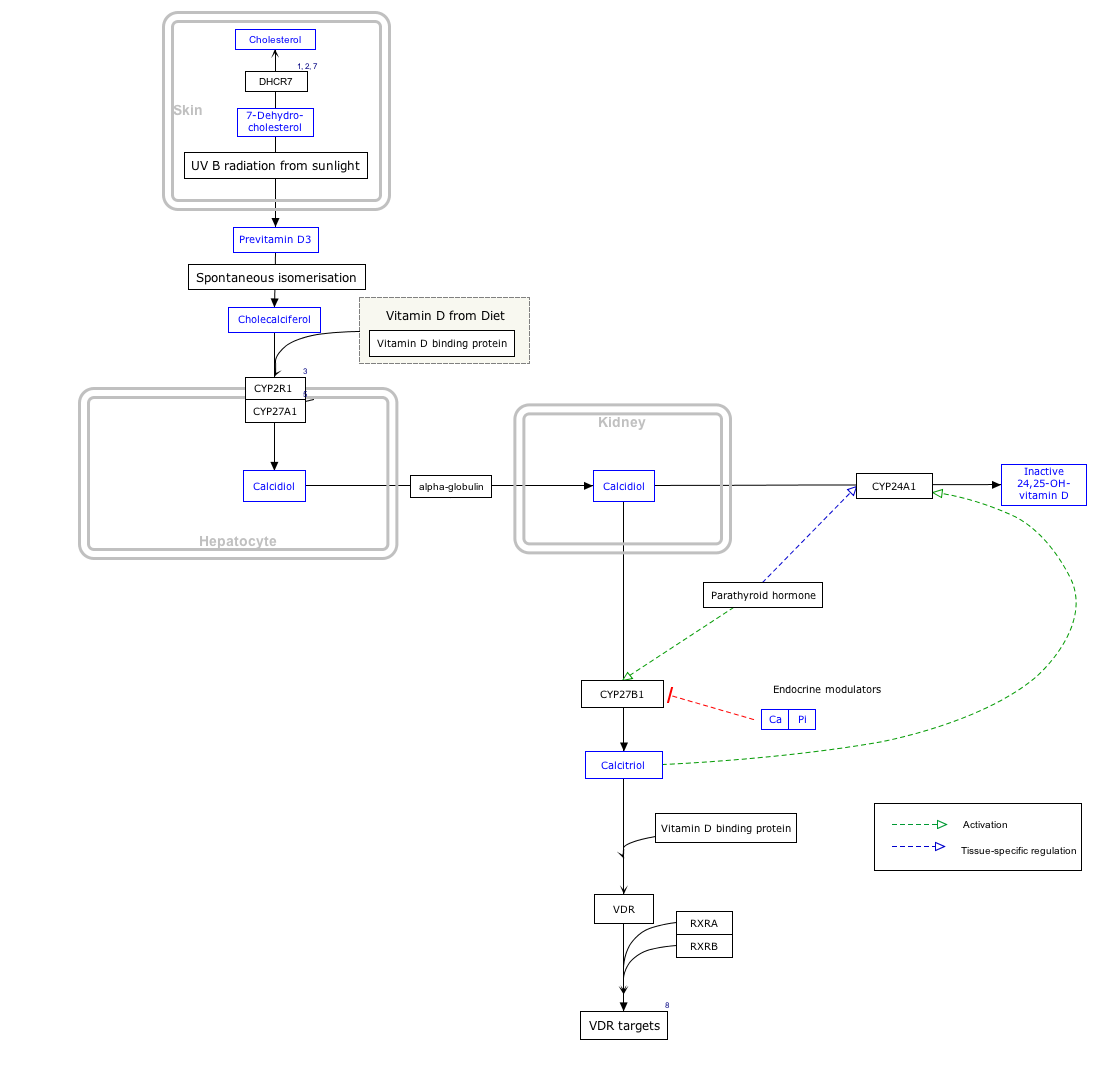
Calcifediol, also known as calcidiol, 25-hydroxycholecalciferol, or 25-hydroxyvitamin D3 (abbreviated 25(OH)D3),[1] is a form of vitamin D produced in the liver by hydroxylation of vitamin D3 (cholecalciferol) by the enzyme vitamin D 25-hydroxylase.[3][4][5] Calcifediol can be further hydroxylated by the enzyme 25(OH)D-1α-hydroxylase, primarily in the kidney, to form calcitriol (1,25-(OH)2D3), which is the active hormonal form of vitamin D.[3][4][5]
Calcifediol is strongly bound in blood by the vitamin D-binding protein.[5] Measurement of serum calcifediol is the usual test performed to determine a person's vitamin D status, to show vitamin D deficiency or sufficiency.[4][5] Calcifediol is available as an oral medication in some countries to supplement vitamin D status.[4][6][7]
Remove ads
Biology
Summarize
Perspective
Calcifediol is the precursor for calcitriol, the active form of vitamin D.[3][4] It is synthesized in the liver, by hydroxylation of cholecalciferol (vitamin D3) at the 25-position.[3] This enzymatic 25-hydroxylase reaction is mostly due to the actions of CYP2R1, present in microsomes, although other enzymes such as mitochondrial CYP27A1 can contribute.[5][8] Variations in the expression and activity of CYP2R1, such as low levels in obesity, affect circulating calcifediol.[8] Similarly, vitamin D2, ergocalciferol, can also be 25-hydroxylated to form 25-hydroxyergocalciferol, (ercalcidiol, 25(OH)D2);[1] both forms are measured together in blood as 25(OH)D.[3][4]
At a typical intake of cholecalciferol (up to 2000 IU/day), conversion to calcifediol is rapid. When large doses are given (100,000 IU), it takes 7 days to reach peak calcifediol concentrations.[9] Calcifediol binds in the blood to vitamin D-binding protein (also known as gc-globulin) and is the main circulating vitamin D metabolite.[4][5] Calcifediol has an elimination half-life of around 15 to 30 days.[4][9]
Calcifediol is further hydroxylated at the 1-alpha-position in the kidneys to form 1,25-(OH)2D3, calcitriol.[3][4] This enzymatic 25(OH)D-1α-hydroxylase reaction is performed exclusively by CYP27B1, which is highly expressed in the kidneys where it is principally regulated by parathyroid hormone, but also by FGF23 and calcitriol itself.[3][5][8] CYP27B1 is also expressed in a number of other tissues, including macrophages, monocytes, keratinocytes, placenta and parathyroid gland and extra-renal synthesis of calcitriol from calcifediol has been shown to have biological effects in these tissues.[8][10]
Calcifediol is also converted into 24,25-dihydroxycholecalciferol by 24-hydroxylation.[3] This enzymatic reaction is performed by CYP24A1 which is expressed in many vitamin D target tissues including kidney, and is induced by calcitriol.[5] This will inactivate calcitriol to calcitroic acid, but 24,25-(OH)2D3 may have some biological actions itself.[5]
Remove ads
Blood test for vitamin D deficiency
Summarize
Perspective
In medical practice, a blood test for 25-hydroxy-vitamin D, 25(OH)D, is used to determine an individual's vitamin D status.[11] The name 25(OH)D refers to any combination of calcifediol (25-hydroxy-cholecalciferol), derived from vitamin D3, and ercalcidiol (25-hydroxy-ergocalciferol),[1] derived from vitamin D2. The first of these (also known as 25-hydroxy vitamin D3) is made by the body, or is sourced from certain animal foods or cholecalciferol supplements. The second (25-hydroxy vitamin D2) is from certain vegetable foods or ergocalciferol supplements.[11] Clinical tests for 25(OH)D often measure the total level of both of these two compounds together, generally without differentiating.[12]
This measurement is considered the best indicator of overall vitamin D status.[11][13][14] US labs generally report 25(OH)D levels as ng/mL. Other countries use nmol/L. Multiply ng/mL by 2.5 to convert to nmol/L.[4]
This test can be used to diagnose vitamin D deficiency, and is performed in people with high risk for vitamin D deficiency, when the results of the test can be used to support beginning replacement therapy with vitamin D supplements.[4][15] Patients with osteoporosis, chronic kidney disease, malabsorption, obesity, and some other infections may be at greater risk for being vitamin D-deficient and so are more likely to have this test.[15] Although vitamin D deficiency is common in some populations including those living at higher latitudes or with limited sun exposure, the 25(OH)D test is not usually requested for the entire population.[15] Physicians may advise low risk patients to take over-the-counter vitamin D supplements in place of having screening.[15]
It is the most sensitive measure, though experts have called for improved standardization and reproducibility across different laboratories.[4][13] According to MedlinePlus, the recommended range of 25(OH)D is 20 to 40 ng/mL (50 to 100 nmol/L) though they recognize many experts recommend 30 to 50 ng/mL (75 to 125 nmol/L).[11] The normal range varies widely depending on several factors, including age and geographic location. A broad reference range of 20 to 150 nmol/L (8-60 ng/mL) has also been suggested,[16] while other studies have defined levels below 80 nmol/L (32 ng/mL) as indicative of vitamin D deficiency.[17]
Increasing calcifediol levels up to levels of 80 nmol/L (32 ng/mL) are associated with increasing the fraction of calcium that is absorbed from the gut.[13] Urinary calcium excretion balances intestinal calcium absorption and does not increase with calcifediol levels up to ~400 nmol/L (160 ng/mL).[18]
Remove ads
Supplementation
Summarize
Perspective
Calcifediol supplements have been used in some studies to improve vitamin D status.[4] Indications for their use include vitamin D deficiency or insufficiency, refractory rickets (vitamin D resistant rickets), familial hypophosphatemia, hypoparathyroidism, hypocalcemia and renal osteodystrophy and, with calcium, in primary or corticosteroid-induced osteoporosis.[19]
Calcifediol may have advantages over cholecalciferol for the correction of vitamin D deficiency states.[6] A review of the results of nine randomized control trials which compared oral doses of both, found that calcifediol was 3.2-fold more potent than cholecalciferol.[6] Calcifediol is better absorbed from the intestine and has greater affinity for the vitamin-D-binding protein, both of which increase its bioavailability.[20] Orally administered calcifediol has a much shorter half-life with faster elimination.[20] These properties may be beneficial in people with intestinal malabsorption, obesity, or treated with certain other medications.[20]
In 2016, the FDA approved a formulation of calcifediol (Rayaldee) 60 microgram daily as a prescription medication to treat secondary hyperparathyroidism in patients with chronic kidney disease.[7]
Interactive pathway map
Click on genes, proteins and metabolites below to link to respective articles. [§ 1]
- The interactive pathway map can be edited at WikiPathways: "VitaminDSynthesis_WP1531".
History
Research in the laboratory of Hector DeLuca identified 25(OH)D in 1968 and showed that the liver was necessary for its formation.[21] The enzyme responsible for this synthesis, cholecalciferol 25-hydroxylase, was isolated in the same laboratory by Michael F. Holick in 1972.[22]
Research
Studies are ongoing comparing the effects of calcifediol with other forms of vitamin D including cholecalciferol in prevention and treatment of osteoporosis.[3][20]
Other Organisms
Teleost Fish
In teleost fish, calcifediol is predominantly converted to calcitriol in the liver, rather than in the kidneys[23] which means circulating levels of calcifediol can be undetectable and alternative measures of vitamin D status are required. There has been some success in using dietary calcifediol supplementation in salmonids to improve growth and food conversion ratio.[24]
References
Wikiwand - on
Seamless Wikipedia browsing. On steroids.
Remove ads