Schizophrenia
psychotic disorder characterized by emotional responsiveness and disintegration of thought process From Wikipedia, the free encyclopedia
Remove ads
Schizophrenia is a mental disorder that is usually diagnosed by a psychiatrist and affects an individual's daily life.[1] For some people, it is a lifelong mental disorder that causes them to behave, feel, or think differently than other people.
The English used in this article or section may not be easy for everybody to understand. (March 2024) |
Schizophrenia can cause psychotic symptoms like hallucinations or delusions. However, not all people with schizophrenia have these symptoms all the time. Schizophrenia can also cause problems with cognition (thinking) and mood.[2]
Schizophrenia is a common disorder, affecting one in 200 people.[3]While it's believed that genetics, environmental, and brain chemistry play a role in such a diagnosis, it's uncertain where schizophrenia originates from.[4] If one child in a family shows clear signs of schizophrenia, there is a higher risk that other family members will have these same symptoms.
People with schizophrenia typically have a higher risk of self-harm compared to the general populations. This might be due to hallucinations, depression, and/or other factors.
Prevention is difficult because there is no reliable way to find out in advance who will get schizophrenia.[5] Attempting to prevent schizophrenia in the pre-onset phase with anti-psychotic drugs is of uncertain benefit and so is not recommended (as of 2009).[6] The British NICE guidelines recommend cognitive behavioural talk therapy for all people at risk.[7]
Schizophrenia is treatable. Many people with the disorder live normal lives with a combination of a therapy and medications.
Schizophrenia and dissociative identity disorder (DID) have some of the same symptoms.[8] Some similar mental illnesses include schizotypal personality disorder, schizoaffective disorder, and schizoid personality disorder.
Remove ads
Name
The word schizophrenia comes from the Greek words, schisma and phren. Literally, it means split mind. [9]
Symptoms
Disorganized thinking
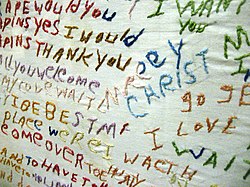
A cloth embroidered by a person with schizophrenia, a written example of a "word salad"; a meaningless mixture of words and phrases.This is one example of the disorganized thinking caused by the disorder.
Emotion-matching task
This task involves picking one of the images at the bottom that expresses the same emotion as the one at top. People with schizophrenia often have difficulty recognizing facial emotions.[10]No medical tests can show that a person has schizophrenia. People are diagnosed based on the symptoms they report and show.
Doctors and psychologists sometimes disagree on whether a person has schizophrenia.[11] For example, lists of schizophrenia's symptoms include wording like "Disorganized [not organized, or oddly organized] speech present for a significant portion of time." It is difficult to agree on what exactly "disorganized speech" is and how disorganized it has to be to receive a diagnosis.
The symptoms of schizophrenia fall into three main categories: positive symptoms, negative symptoms, and cognitive symptoms.[12]
Positive symptoms
Positive symptoms are thoughts, behaviors, or anything experienced by the senses that are not shared by others - like hearing voices that are not really there. They are called 'positive' not because they are good, but because they are added.
These symptoms may include:[13]
- Having strange thoughts that do not make sense (delusions)
- Having difficulty organizing thoughts and speech
- Feeling, hearing, seeing, smelling, or tasting things that do not exist (hallucinations).
A person can also have these symptoms if they have stopped taking anti-psychotic or anti-vomiting medicines too quickly.[14]
Positive symptoms often decrease with drug treatment[15] and cognitive behavioral therapy (CBT).[16]
Delusions and hallucinations
People with schizophrenia often have delusions or hallucinations. As estimated by the IPSS, about 70% of schizophrenic individuals experience hallucinations.[17]
Negative symptoms
A person is having negative symptoms when they do not have thoughts, behaviors or emotions that healthy people have. For example:
- They do not show any emotion on their face (they have a "flat affect")
- They speak slowly, using very short words (they have "monosyllabic speech")
- They move very little or do not use gestures
- They cannot feel pleasure
- They do not feel interested in anything, including other people
- Being unable to act spontaneously (without planning first)
Negative symptoms, as the name suggests, essentially "take away" from life and day-to-day interactions, making it harder for people with schizophrenia to have meaningful relationships with the people around them.
If a person is having negative symptoms, they do not necessarily have schizophrenia. These can also be:[14]
- Symptoms of depression, bipolar disorder, or other mental health disorders
- Side effects of medications like antipsychotics, antidepressants, sleep medications, and anti-anxiety medications
- Symptoms of medical problems, like hypothyroidism or low metabolism
Cognitive symptoms (or cognitive deficits)
Cognitive symptoms can include:[14]
- Problems paying attention
- Not remembering things
- Not having a concept of time
- Being unable to plan and organize
Of all of schizophrenia's symptoms, cognitive symptoms are the most disabling because they affect day-to-day activities. Also, it can be difficult to recognize them as part of the disorder.
Like with negative symptoms, a person does not necessarily have schizophrenia if they are having cognitive symptoms. Cognitive symptoms can also be:[14]
- Symptoms of depression, ADHD, or other mental health disorders
- Side effects of medications like antipsychotics, antidepressants, sleep medications, and anti-anxiety medications
- Symptoms of medical problems, like dementia
Remove ads
Risk factors/causes

There are many risk factors that can increase a person's chances of developing schizophrenia.
They include trauma (damage caused by stressful events) and genetics (schizophrenia running in families). Having a schizophrenic parent may be very stressful, and there may also be genes that influence the development of schizophrenia.
It is very easy to show that trauma, such as sexual abuse (forced unwanted sexual behaviour towards somebody), increases the risk, but 40 years of searching for the right genes has not found anything that has been confirmed by independent research groups.[18]
Inherited factors
A combination of what has happened to a person and the person’s genes may play a role in the development of schizophrenia.[19][20]
People who have family members with schizophrenia and who experienced a brief period of psychotic symptoms have a 20 to 40 percent chance of being diagnosed one year later. This may be both the result of stressful events because of the family member and possibly a genetic effect.[21]
It is difficult to know if schizophrenia is inherited because it is hard to find out whether something comes from genes or the environment.[22] Those who have a parent, a brother or sister with schizophrenia have a higher risk of developing schizophrenia. The risk is even higher if one has an identical twin with schizophrenia.[20] This may seem to show that schizophrenia is inherited. However, it may be the stress of living with a schizophrenic family member that is traumatic.
Identical twins are much closer and are treated much more in the same way, and this may be the reason why one of them is more likely to get schizophrenia if the other has it. Dr. Jay Joseph has found many problems with the scientific studies of inheriting schizophrenia, including false reporting of results. Joseph also claims that 40 years of the search for the schizophrenia gene has not found a single gene that independent research groups have confirmed.[18][23]
Environmental factors
There are may environmental risk factors factors for schizophrenia. These include:[19][20][24][25]
- Drug use
- Stress before birth
- In some cases, being exposed to infectious diseases (diseases that spread from person to person)
- Living in a city during childhood or as an adult (this has been found to double the risk of schizophrenia[19][20] - even after taking into account drug use, race, and the size of one's social group)[26]
- Whether the person feels socially isolated
- Social adversity like racial discrimination (treating a person badly because of their race)
- Conflict in the person's family
- Unemployment
- Poor housing conditions
- Childhood abuse
- Trauma
Substance abuse
Several drugs have been linked with the development of schizophrenia and the abuse (harmful use) of certain drugs can cause symptoms like those of schizophrenia.[20][20][27] About half of those people who have schizophrenia use too much drugs or alcohol, possibly to deal with depression, anxiety, boredom, or loneliness.[28] Frequent marijuana use may double the risk of serious mental illness, including schizophrenia.[29]
Smoking
A study made during 2019 found that approximately 80% of the sample group of surveyed individuals with a diagnosis of schizophrenia consumed tobacco.[30]
Pre-birth factors
Factors such as lack of oxygen, infection, or stress and lack of healthy foods in the mother during pregnancy might result in a slight increase in the risk of schizophrenia later in life.[19] People who have schizophrenia are more likely to have been born in winter or spring (at least in the northern half of the world). This might relate to increased rates of exposures to viruses before birth.[20][31]
Brain structure

Some people who have schizophrenia have differences in their brain structure compared to those who do not have the disorder. These differences are often in the parts of the brain that manage memory, organization, emotions, the control of impulsive behavior, and language.[32] For example, there is less brain volume in the frontal cortex and temporal lobes, and problems within the corpus callosum, the band of nerve fibers which connects the left side and the right side of the brain. People with schizophrenia also tend to have larger lateral and third ventricles. The ventricles are spaces within the brain filled with cerebrospinal fluid.[33]
Brain neurons
It is believed that there are problems with the brain's neurons in schizophrenia.
Remove ads
Diagnosis
The DSM-IV-TR or the ICD-10 criteria are used to determine whether a person has schizophrenia.[19] These criteria use the self-reported experiences of the person and reported abnormalities (unusual occurrences) in the behavior of the person, followed by a clinical assessment. A person can be determined to have the disease only if the symptoms are severe.[20]
Differential diagnosis
There are various medical conditions, other psychiatric conditions and drug abuse related reactions that may mimic the symptoms of schizophrenia (meaning they have some or all of the same symptoms). For example, delirium can cause visual hallucinations, or an unpredictable changing levels of consciousness. Schizophrenia occurs along with obsessive-compulsive disorder (OCD), a disorder in which a person becomes obsessed with certain ideas or actions. However, separating the obsessions of OCD from the delusions of schizophrenia can be difficult.[37]
People with schizophrenia may also have other mental health disorders, like depression, anxiety and drug abuse.[38]
Remove ads
Treatment
Treatment of schizophrenia may include medication to help treat the symptoms, different types of psychotherapy (therapy by a professional), such as cognitive-behavioral therapy and many rehabilitation therapies (therapies restoring things to how they were before), such as cognitive remediation therapy. Cognitive behavioral therapy, CBT, is a talk therapy that focuses on helping the person to think about their strange ideas (delusions) in more realistic ways.
The therapist may design a behavioral experiment for paranoia (false beliefs of danger) that will help the person to find out for example, if there really are cameras everywhere in the house. For hallucinations, cognitive therapy focuses on normalizing: many people hear voices without being stressed, and we all hear voices in the form of thoughts, it is just that people with schizophrenia hear them a bit more clearly than most people.[16]
A 2006 survey of 941 patients from 7 studies found no clear evidence that treating schizophrenia with anti-psychotic drugs early is effective.[39] There is some evidence which shows that early treatment with drugs improves short term outcomes for people who have a serious episode of mental illness. These measures show little benefit five years later.[19]

Some of the goals during the acute phase of treatment are to prevent harm. To prevent harm, the person being treated will have the severity of psychosis and it's symptoms reduced. These symptoms include agitation, aggression, negative symptoms, self-disorder, and thought disorders.[40]
Medication
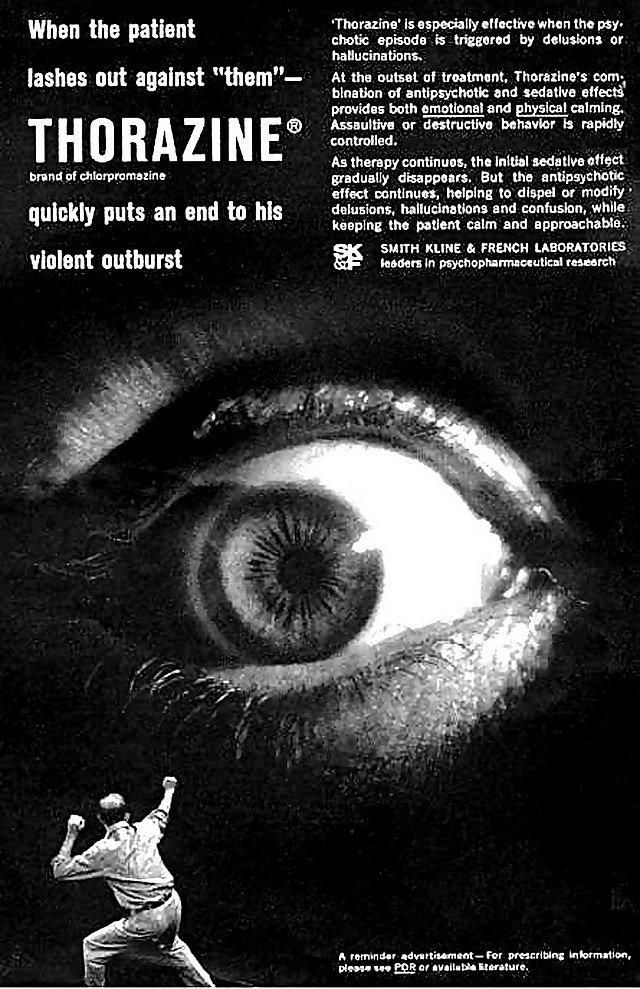
The first-line psychiatric treatment for schizophrenia is antipsychotic medication,[7] which can reduce the positive symptoms in about seven to fourteen days. However, medication fails to improve negative symptoms or problems in thinking significantly.[41][42]
Some reviews of research sponsored by the makers of antipsychotic drugs claim that about 40 to 50 percent of people have a good response to medication, 30 to 40 percent have a partial response, and 20 percent have an unsatisfactory response (after 6 weeks on two or three different drugs).[41] Other research from The British Journal of Psychiatry were more negative and claimed that "the clinical relevance of antipsychotics is in fact limited." This study included 22 428 patients and 11 antipsychotic drugs.[43] A drug called clozapine is an effective treatment for people who respond poorly to other drugs, but clozapine can lower the white blood cell count in 1 to 4 percent of people who take it. This is a serious side effect.[19][20][44]
For people who are unwilling or unable to take drugs regularly, injectable long-acting preparations of antipsychotics can be used.[45] When used in combination with mental and social interventions (treatment), such preparations can help people to continue their treatment.[45]
In Western countries, where medications are used as treatment, 1 of 3 get well, but many suffer from drug side effects such as diabetes, obesity, and brain damage.[46]
Psychosocial therapies
Numerous mental and social interventions can be useful in treating schizophrenia. Such interventions include various types of therapy,[47] community-based treatments, supported employment, skills training, token economic interventions, and mental interventions for drug or alcohol use and weight management.[48] Family therapy or education, which addresses the whole family system of an individual, might reduce a return of symptoms or the need for hospitalizations (having to go into hospital.)[47] There is growing evidence for the effectiveness of cognitive behavioral therapy (also known as “talk therapy”) .[49][50]
The British national guidelines for treatment (NICE) recommend for both people are at risk of getting schizophrenia and people who have got it, cognitive behavioral therapy (CBT) and family therapy. Getting support from people who have become well from schizophrenia is also strongly recommended. [51] In a family oriented treatment program in Finland, Open Dialog, 8 out of 10 people with schizophrenia get well with no medication or very limited drug use, often only anxiety medication.[52]
Official guidelines
The British national guidelines for treatment (NICE) suggest the following:
- Check for reactions to traumatic experiences
- Decide together with a doctor about using medication, taking into account the side effect risk of getting diabetes, becoming seriously overweight, getting brain damage (tardive dyskinesia, 5% risk pr year), men growing breasts, and feelings described as inner torture (akathesia).
The guidelines also warn against using more than one antipsychotic drug at the same time. Both for people who are at risk for getting schizophrenia and for people who have got it, they recommend cognitive behavioral therapy (CBT) and family therapy. Getting support from people who have become well from schizophrenia is also strongly recommended. [51] In a family oriented treatment program in Finland, Open Dialog, 8 out of 10 people with schizophrenia get well with no medication or very limited drug use, often only with anxiety medication.[52]
Hope
In a family treatment called "Open dialog" in Finland, eight out of every ten people with schizophrenia "get well." In developing countries, where doctors use less drugs, 2 out of 3 patients get well from schizophrenia.[46]
Remove ads
Outlook
Schizophrenia has great human and economic costs.[19] The condition results in a decreased life expectancy of 12 to 15 years, primarily because of its association with being overweight, not exercising, and smoking cigarettes. An increased rate of suicide (a person killing themself) plays a lesser role.[19] These differences in life expectancy increased between the 1970s and 1990s.[53]
Schizophrenia is a major cause of disability, with active psychosis ranked as the third-most-disabling condition.[54] Approximately three-fourths of people with schizophrenia have an ongoing disability with symptoms that keep coming back.[41] Some people do recover completely and others function well in society.[55] Most people with schizophrenia live independently, with community support.[19] In people with a first episode of serious mental symptoms, 42 percent have a good long-term outcome, 35 percent have an intermediate outcome and 27 percent have a poor outcome.[56] Outcomes for schizophrenia appear better in the developing world than in the developed world,[57] although that conclusion has been questioned.[58][59]
The suicide rate of people who have schizophrenia is estimated to be about 4.9 percent, most often occurring in the period following the first appearance of symptoms or the first hospital admission.[60] 20 to 40 percent try to kill themselves at least once.[61][62]
Schizophrenia and smoking have shown a strong association in studies worldwide.[63][64] Use of cigarettes is especially high in individuals who have schizophrenia, with estimates ranging from 80 to 90 percent of these people being regular smokers, compared to 20 percent of the general population.[64] Those individuals who smoke tend to smoke heavily and to smoke cigarettes with a high nicotine content.[62]
Research continues on schizophrenia. In the spring of 2013, genetics associations were shown between five major psychiatric disorders: autism, ADHD, bipolar disorder, depression, and schizophrenia per recent study.[65][66] In the summer of 2013, for the first time, brain tissue development was replicated in three dimensions by scientists cloning a human "mini-brain" using stem cells. This could help with schizophrenia and autism neurological research (research related to the brain.) [67]
Remove ads
Likelihood
As of 2011, schizophrenia affects around 0.3% to 0.7% of people,[19] or 24 million people worldwide,[68] at some point in their lives. More men are affected than women: the number of males with the disorder is 1.4 times greater than that of females. Schizophrenia usually appears earlier in men.[20] For males the symptoms usually start from 20 to 28 years of age, and in females it is 26 to 32 years of age.[69] Symptoms that start in childhood,[70] middle or old age are much rarer.[71] Despite the received wisdom that schizophrenia occurs at similar rates worldwide, its rate of likelihood varies across the world,[72] within countries,[73] and at the local level.[74] The disorder causes approximately 1% of worldwide disability adjusted life years (in other words, years spent with a disability).[20] The rate of schizophrenia varies depending on how it is defined.[19]
Remove ads
History

Accounts of a schizophrenia-like syndrome are rare before the 19th century. Detailed case reports from 1797 and 1809, are regarded as the earliest cases of the disorder.[76] Schizophrenia was first described as a distinct syndrome affecting teenagers and young adults by Bénédict Morel in 1853, termed démence précoce (literally 'early dementia'). The term dementia praecox was used in 1891 by Arnold Pick in a case report of a psychotic disorder. In 1893 Emil Kraepelin introduced a new distinction in the classification of mental disorders between dementia praecox and mood disorder (termed manic depression and including both unipolar and bipolar depression). Kraepelin believed that dementia praecox was primarily a disease of the brain,[77] and a form of dementia, different from other forms of dementia such as Alzheimer's disease which usually happen later in life.[78]
Eugen Bleuler made the word "schizophrenia," which means "split mind,"[79] in 1908. The word was intended to describe the separation of functioning between personality, thinking, memory, and perception.[80]
In the early 1970s, the criteria for determining schizophrenia were the subject of numerous controversies. Schizophrenia was diagnosed far more often in the United States than in Europe.[81] This difference was partly the result of looser criteria for determining whether someone had the condition in the United States, where the DSM-II manual was used. In Europe, the ICD-9 manual was used. A 1972 study, published in the journal Science, concluded that the diagnosis of schizophrenia in the United States was often unreliable.[82] These factors resulted in the publication of the DSM-III in 1980 with a stricter and more defined criteria for the diagnosis.[83]
Remove ads
Society and culture

Negative social judgment has been identified as a major obstacle in the recovery of people who have schizophrenia.[84]
In 2002, the term for schizophrenia in Japan was changed from "Seishin-Bunretsu-Byō" 精神分裂病 ("mind-split-disease") to "Tōgō-shitchō-shō" 統合失調症 ("integration disorder"), to put less shame and embarrassment with schizophrenia.[85] Because people understood that the disease is caused by many things (not just one mental cause), they gave it this new name. During the three years after the name change, the percentage of people who were informed of the diagnosis changed from 37 percent to 70 percent.[86]
In the United States in 2002, the cost of schizophrenia, including direct costs (people who were not hospitalized, people who were hospitalized, medicines, and long-term care) and non-healthcare costs (law enforcement, reduced workplace productivity, and unemployment), was estimated to be $62.7 billion.[87]
The book “A Beautiful Mind” and the film of the same name are about the life of John Forbes Nash, an American mathematician and Nobel Prize winner who has schizophrenia. The movie “The Soloist” is based on the life of Nathaniel Ayers, a gifted musician who dropped out of the Julliard School, in New York City after the symptoms of schizophrenia began. He later became homeless in Los Angeles, California, in the notorious Skid Row section.

Related pages
References
Wikiwand - on
Seamless Wikipedia browsing. On steroids.
Remove ads