Loading AI tools
Medical condition From Wikipedia, the free encyclopedia
Neonatal jaundice is a yellowish discoloration of the white part of the eyes and skin in a newborn baby due to high bilirubin levels.[1] Other symptoms may include excess sleepiness or poor feeding.[1] Complications may include seizures, cerebral palsy, or kernicterus.[1]
| Neonatal jaundice | |
|---|---|
| Other names | Neonatal hyperbilirubinemia, neonatal icterus, jaundice in newborns |
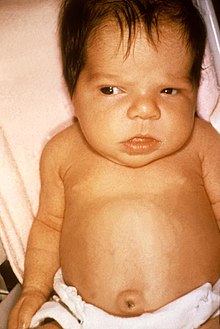 | |
| Jaundice in a newborn | |
| Specialty | Pediatrics |
| Symptoms | Yellowish discoloration of the skin and white part of the eyes[1] |
| Complications | Seizures, cerebral palsy, kernicterus[1] |
| Usual onset | Newborns[1] |
| Types | Physiologic, pathologic[1] |
| Causes | Red blood cell breakdown, liver disease, infection, hypothyroidism, metabolic disorders[2][1] |
| Diagnostic method | Based on symptoms, confirmed by bilirubin[1] |
| Treatment | More frequent feeding, phototherapy, exchange transfusions[1] |
| Frequency | >50% of babies[1] |
In most of cases there is no specific underlying physiologic disorder.[2] In other cases it results from red blood cell breakdown, liver disease, infection, hypothyroidism, or metabolic disorders (pathologic).[2][1] A bilirubin level more than 34 μmol/L (2 mg/dL) may be visible.[1] Concerns, in otherwise healthy babies, occur when levels are greater than 308 μmol/L (18 mg/dL), jaundice is noticed in the first day of life, there is a rapid rise in levels, jaundice lasts more than two weeks, or the baby appears unwell.[1] In those with concerning findings further investigations to determine the underlying cause are recommended.[1]
The need for treatment depends on bilirubin levels, the age of the child, and the underlying cause.[1][3] Treatments may include more frequent feeding, phototherapy, or exchange transfusions.[1] In those who are born early more aggressive treatment tends to be required.[1] Physiologic jaundice generally lasts less than seven days.[1] The condition affects over half of babies in the first week of life.[1] Of babies that are born early about 80% are affected.[2] Globally over 100,000 late-preterm and term babies die each year as a result of jaundice.[4]
Bronze baby syndrome (dark pigmentation of skin).
The primary symptom is yellowish discoloration of the white part of the eyes and skin in a newborn baby.[1] Other symptoms may include excess sleepiness or poor feeding.[1]
A bilirubin level more than 34 μmol/L (2 mg/dL) may be visible.[1] For the feet to be affected level generally must be over 255 μmol/L (15 mg/dL).[1]
Prolonged hyperbilirubinemia (severe jaundice) can result in chronic bilirubin encephalopathy (kernicterus).[5][6] Quick and accurate treatment of neonatal jaundice helps to reduce the risk of neonates developing kernicterus.[7]
Infants with kernicterus may have a fever[8] or seizures.[9] High pitched crying is an effect of kernicterus.[citation needed]
Exchange transfusions performed to lower high bilirubin levels are an aggressive treatment.[10]
In newborns, jaundice tends to develop because of two factors—the breakdown of fetal hemoglobin as it is replaced with adult hemoglobin and the relatively immature metabolic pathways of the liver, which are unable to conjugate and so excrete bilirubin as quickly as an adult. This causes an accumulation of bilirubin in the blood (hyperbilirubinemia), leading to the symptoms of jaundice.[citation needed]
If the neonatal jaundice is not resolved with simple phototherapy, other causes such as biliary atresia, Progressive familial intrahepatic cholestasis, bile duct paucity, Alagille syndrome, alpha 1-antitrypsin deficiency, and other pediatric liver diseases should be considered. The evaluation for these will include blood work and a variety of diagnostic tests. Prolonged neonatal jaundice is serious and should be followed up promptly.[11]
Severe neonatal jaundice may indicate the presence of other conditions contributing to the elevated bilirubin levels, of which there are a large variety of possibilities (see below). These should be detected or excluded as part of the differential diagnosis to prevent the development of complications. They can be grouped into the following categories:
| Neonatal jaundice | |||||||||||||||||||||||||||||||||||||||||||||||
| Unconjugated bilirubin | Conjugated bilirubin | ||||||||||||||||||||||||||||||||||||||||||||||
| Pathologic | Physiological jaundice of neonates | Hepatic | Post-hepatic | ||||||||||||||||||||||||||||||||||||||||||||
| Hemolytic | Non-hemolytic | ||||||||||||||||||||||||||||||||||||||||||||||
| Intrinsic causes | Extrinsic causes | ||||||||||||||||||||||||||||||||||||||||||||||
"Breastfeeding jaundice" (or "lack of breastfeeding jaundice") is caused by insufficient breast milk intake,[13] resulting in inadequate quantities of bowel movements to remove bilirubin from the body. This leads to increased enterohepatic circulation, resulting in increased reabsorption of bilirubin from the intestines.[14] Usually occurring in the first week of life, most cases can be ameliorated by frequent breastfeeding sessions of sufficient duration to stimulate adequate milk production.[15]
Whereas breastfeeding jaundice is a mechanical problem, breast milk jaundice is a biochemical occurrence and the higher bilirubin possibly acts as an antioxidant. Breast milk jaundice occurs later in the newborn period, with the bilirubin level usually peaking in the sixth to 14th days of life. This late-onset jaundice may develop in up to one third of healthy breastfed infants.[16]
Most infants develop visible jaundice due to elevation of unconjugated bilirubin concentration during their first week. This is called physiological jaundice. This pattern of hyperbilirubinemia has been classified into two functionally distinct periods.[21]
Mechanisms involved in physiological jaundice include:
Diagnosis is often by measuring the serum bilirubin level in the blood.[3] In those who are born after 35 weeks and are more than a day old transcutaneous bilirubinometer may also be used.[3] The use of an icterometer, a piece of transparent plastic painted in five transverse strips of graded yellow lines, is not recommended.[3]
This is hand held, portable and rechargeable but expensive. When pressure is applied to the photoprobe, a xenon tube generates a strobe light, and this light passes through the subcutaneous tissue. The reflected light returns through the second fiber optic bundle to the spectrophotometric module. The intensity of the yellow color in this light, after correcting for the hemoglobin, is measured and instantly displayed in arbitrary units.[citation needed]
Any of the following features suggests pathological jaundice:[citation needed]
The signs which help detect pathological jaundice are the presence of intrauterine growth restriction, stigma of intrauterine infections (e.g. cataracts, small head, and enlargement of the liver and spleen), cephalohematoma, bruising, signs of bleeding in the brain's ventricles. History of illness is noteworthy. Family history of jaundice and anemia, family history of neonatal or early infant death due to liver disease, maternal illness suggestive of viral infection (fever, rash or lymphadenopathy), maternal drugs (e.g. sulphonamides, anti-malarials causing red blood cell destruction in G6PD deficiency) are suggestive of pathological jaundice in neonates.[citation needed]
The bilirubin levels for initiative of phototherapy varies depends on the age and health status of the newborn. However, any newborn with a total serum bilirubin greater than 359 μmol/L ( 21 mg/dL) should receive phototherapy.[25]

Babies with neonatal jaundice may be treated with colored light called phototherapy, which works by changing trans-bilirubin into the water-soluble cis-bilirubin isomer.[26][27][28]: 2533
The phototherapy involved is not ultraviolet light therapy but rather a specific frequency of blue light. The light can be applied with overhead lamps, which means that the baby's eyes need to be covered, or with a device called a biliblanket, which sits under the baby's clothing close to its skin.[27]
The use of phototherapy was first discovered, accidentally, at Rochford Hospital in Essex, England, when a nurse, Sister Jean Ward, noticed that babies exposed to sunlight had reduced jaundice, and a pathologist, Dr. Perryman, who noticed that a vial of blood left in the sun had turned green. Drs Cremer, Richards and Dobbs put together these observations,[29] leading to a landmark randomized clinical trial which was published in Pediatrics in 1968; it took another ten years for the practice to become established.[27][30] Massage therapy could be useful in addition to phototherapy in order to reduce the phototherapy duration. However, it does not appear to reduce the requirement for phototherapy in the treatment of neonatal jaundice.[31]
Recent studies from several countries show that phototherapy can safely and effectively be performed in the family's home, and since 2022 home phototherapy is recommended as an alternative to readmission to hospital in the American national guidelines.[32][33][34] However, there have been several reports about the possible relationship between neonatal phototherapy and the increased risk of future cancer. A recent systematic review has found that there may be a statistically significant association between phototherapy and various hematopoietic cancers (especially myeloid leukemia).[35]
Much like with phototherapy the level at which exchange transfusion should occur depends on the health status and age of the newborn. It should however be used for any newborn with a total serum bilirubin of greater than 428 μmol/L ( 25 mg/dL ).[25][28]: 2533
Penicillamine was studied in the 1970s in hyperbilirubinemia due to ABO hemolytic disease.[36] While tin mesoporphyrin IX may decrease bilirubin such use is not recommended in babies.[36] Preclinical studies have looked at minocycline to help prevent neurotoxicity.[36] Clofibrate may decrease the duration of phototherapy.[36] Evidence as of 2012 however is insufficient to recommend its use.[37]
Seamless Wikipedia browsing. On steroids.
Every time you click a link to Wikipedia, Wiktionary or Wikiquote in your browser's search results, it will show the modern Wikiwand interface.
Wikiwand extension is a five stars, simple, with minimum permission required to keep your browsing private, safe and transparent.