Diabetes management
Management of diabetes From Wikipedia, the free encyclopedia
Diabetes Mellitus is a metabolic disease that is characterized by chronic hyperglycemia. Therefore, the main goal of diabetes management is to keep blood glucose (BG) levels as normal as possible.[1] If diabetes is not well controlled, further challenges to health may occur.[1] People with diabetes can measure blood sugar by various methods, such as with a BG meter or a continuous glucose monitor (CGM), which monitors over several days.[2] Glucose can also be measured by analysis of a routine blood sample.[2] In addition to lifestyle modification, some individuals may need medications to adequately control their blood sugar levels. Other goals of diabetes management are to prevent or treat complications that can result from the disease itself and from its treatment.[3]
Description
Summarize
Perspective
Diabetes is a chronic disease and it is important to have control of the diabetes as it can cause many complications. Diabetes can cause acute problems such as too low (hypoglycemia) or high blood sugar (hyperglycemia). Diabetes affects the blood vessels in the body, such as capillaries and arteries, which are the routes blood take to deliver nutrients and oxygen to the organs in the body.[4] By affecting the blood flow, diabetes increases the risk of other conditions such as strokes and heart disease (heart attacks).[2] Diabetes also affects small blood vessels, such as capillaries, in organs such as the eyes and the kidneys to cause diabetic retinopathy and diabetic nephropathy, respectively.[4]
Therefore, it becomes important to lower the sugar levels in the body in addition to control other risk factors that also contribute to the major complications such as smoking, alcohol use, excessive weight, high blood pressure, and high cholesterol.[1] Often, the recommended treatment is a combination of lifestyle changes such as increasing exercise and healthy eating, along with medications to help control the BG levels in the long term.[2] In addition to management of the diabetes, patients are recommended to have routine follow up with specialist to manage possible common complications due to the diabetes such as foot ulcers, vision changes, and hearing loss.[5]
Measurement
There are several methods in which blood sugar is measured including with a glucose meter, continuous glucose monitor and routine bloodwork.

The glucose meter (as seen in image 2) is a common a simple method in which glucose levels can be measured at home or in a clinical setting and is usually done several times per day. The test works by taking a small blood sample of blood using a lancet (a sterile pointed needle) to prick a finger (Image 1). The blood droplet is usually collected at the bottom of a test strip, while the other end is inserted in the glucose meter.[6] The drop of blood is drawn into the meter and can directly measure the glucose in the sample. The units of blood sugar level from a glucose meter, with the result either in mg/dL (milligrams per deciliter in the US) or mmol/L (millimoles per liter in Canada and Eastern

Europe) of blood.[7] Control of diabetes may be improved by patients using home glucose meters to regularly measure their glucose levels.[8]

Continuous glucose monitors are another method to measure BG levels. A CGM is a device that sits on the surface of the skin and measures the amount of glucose between the cells with a probe. The device does not directly measure the blood sugar but calculates it based on the sample of the measurements it takes from the probe.[7] The device will report the glucose level continuously and usually it has an alarm that will alert patients if the glucose level is too high or low.[7] The device also is able to graph the glucose readings over the time the sensor was in use and is very useful for adjusting treatment.[7]
In addition to the above tests, glucose can be measured on routine labs. One common test ordered by healthcare providers is a Basic Metabolic Panel (BMP) which is a blood test that looks at several different substances in the body, including BG.[9] People are told to fast for 8 hours before drawing the labs so that the provider can see the fasting glucose level.[2] The normal level for fasting blood sugar in non-diabetic patients is 70 to 99 mg/dL (3.9 and 5.5 mmol/L).
Another useful test that has usually done in a laboratory is the measurement of blood HbA1c (hemoglobin A1c) levels. In the blood, there is a molecule called hemoglobin which carries oxygen to the cells. Glucose can attach itself to this molecule and if the BG is consistently high, the value of the A1c will go up. This test, unlike the other tests, is measured as a percentage because the test measure the proportion of all the hemoglobin that has glucose attached.[2][10] This test measures the average amount of diabetic control over a period of about 3 months.[10] In non-diabetic people, the HbA1c level ranges from 4.0 to 5.7%.[10] Regular 6 monthly laboratory testing of HbA1c (glycated hemoglobin) provides some assurance of long-term control and allows the adjustment of the patient's routine medication dosages in such cases.
Optimal management of diabetes involves people measuring and recording their own BG levels. By keeping a diary of their own BG measurements and noting the effect of food and exercise, patients can modify their lifestyle to better control their diabetes. For people on insulin, involvement is important in achieving effective dosing and timing.
Glycemic control
Glycemic control is a medical term referring to the typical levels of BG in a person with diabetes mellitus. Much evidence suggests that many of the long-term complications of diabetes, result from many years of hyperglycemia (elevated levels of glucose in the blood).[11]
"Perfect glycemic control" would mean that glucose levels were always normal (70–130 mg/dL or 3.9–7.2 mmol/L) and indistinguishable from a person without diabetes. Good glycemic control, in the sense of a "target" for treatment, has become an important goal of diabetes care. Poor glycemic control refers to persistently (over several months) elevated BG in the 200 to 500 mg/dL (11–28 mmol/L). This is also measured by Hb A1c levels, which may range from greater than 9%.
Goals
They are suggested in clinical practice guidelines released by various national and international diabetes organizations.[12][13]
The targets are:
- HbA1c of less than 6% or 7.0% if they are achievable without significant hypoglycemia[14][15]
- Preprandial (before eating) BG: 3.9 to 7.2 mmol/L (70 to 130 mg/dL)[14]
- 2-hour postprandial (after eating) BG: <10 mmol/L (<180 mg/dL)[14]
Goals should be individualized based on:[14]
- Duration of diabetes
- Age/life expectancy
- Comorbidity
- Known cardiovascular disease or advanced microvascular disease
- Hypoglycemia awareness
In older patients, clinical practice guidelines by the American Geriatrics Society recommend, in frail patients who have a life expectancy of less than 5 years, a target a Hb A1c of 8% is appropriate as the risk of very low blood sugar outweighs the long term benefits of a lower A1c.[16]
Studies have been done to compare the effects of tight vs. conventional, or more relaxed, glycemic control in type 2 diabetics. It shows than to demonstrate a difference in all-cause cardiovascular death, non-fatal stroke, or limb amputation, but decreased the risk of nonfatal heart attack by 15%.[17] Additionally, tight glucose control decreased the risk of progression of kidney, nerve and eye complications, but increased the risk of hypoglycemia.[17]
Lifestyle modification
Summarize
Perspective
Diet
There are many diets that are effective at managing diabetes and it is important that patients understand that there is no one diet that all patients should use.[18] Some diets that have commonly been used successfully in diabetes management and help with weight loss include Mediterranean, vegetarian, low carb or carb-controlled.[18] It is recommended that patients choose a diet that the patient can adhere to in the long run as a diet that is very ideal is impractical if the patient has trouble following it.[18]
A regular diet that has reduced variability in carbohydrates is an important factor in producing normal blood sugars. Patients with diabetes should eat preferably a balanced and healthy diet. Meals should consist of half a plate of non-starchy vegetables, 1/4 plate of lean protein, and 1/4 plate of starch/grain.[18] Patients should avoid excess simple carbs or added fat (such as butter, salad dressing) and instead eat complex carbohydrates such as whole grains.[1] In the long term, it is helpful to eat a consistent diet and amount of carbohydrate to make blood sugar management easier.[19] It is important for patients to eat 3 meals a day as well in order to reduce the chances of hypoglycemia, especially with patients that take insulin.[1]
There is a lack of evidence of the usefulness of low-carbohydrate dieting for people with type 1 diabetes (T1D).[20] Although for certain individuals it may be feasible to follow a low-carbohydrate regime combined with carefully managed insulin dosing, this is hard to maintain and there are concerns about potential adverse health effects caused by the diet.[20] In general people with T1D are advised to follow an individualized eating plan rather than a pre-decided one.[20]
Exercise
Along with diet, exercise is also important for the management of diabetes.[21] Not only does exercising regularly help manage blood sugar levels and weight, it helps reduce the risk of heart attack and stroke, reduces cholesterol levels, reduces risk of diabetes related complications, increases the effect of insulin, provides a boost in energy levels, helps reduce stress, and contributes to positive self-esteem.[22] By exercising, the body becomes more sensitive to insulin, allowing for better absorption of glucose by the muscle cells, for up to 24 hours after exercise.[23] Therefore, an ongoing exercise program is required to maintain the health benefits associated with exercising.[24]
In patients with type 2 diabetes (T2D), the combination of aerobic (cardio) exercise and strength training, as recommended by the American Diabetes Association (ADA) guidelines, is the most effective when it comes to controlling glucose and cholesterol.[25] Aerobic exercise has been shown to largely improve HbA1c, and contributes to weight loss and the enhanced regulation of cholesterol and lipoproteins.[24] This may be any form of continuous exercise that elevates breathing and heart rate such as walking, swimming, or dancing.[26] During the last 20 years, resistance training has gained considerable recognition as an optimal form of exercise for patients with type two diabetes.[24] By building muscle strength, strength training was linked to a 10% to 15% increase in strength, Bone Mineral Density, insulin sensitivity, muscle mass and decrease in blood pressure.[24]
Several studies have made it clear that exercise helps with blood sugar control and has shown to lower HbA1c levels by approximately 0.6% in patients with T2D. The ADA recommends 150 minutes of moderate to vigorous aerobic exercise a week spread over 3 to 7 days with no more than 2 day break between days. Moreover, patients should also pair the aerobic exercise with 2 to 3 nonconsecutive sessions of strength training.
In T1D, there also have been studies that show that, in children and adolescent, there is an association between exercise and lower HB A1c.[27] Furthermore, studies have shown that the longer the length of the exercise program, there is a further reduction in the HB A1c and patients have less insulin requirements.[27] Although the population of these studies are limited to patients under the age of 18, exercise is beneficial in managing diabetes, whether its type 1 or 2.[2] There are many benefits of exercise such as a decreased risk of cardiovascular diseases, including blood pressure, lipid profiles, body composition and insulin sensitivity.[28]
Weight loss
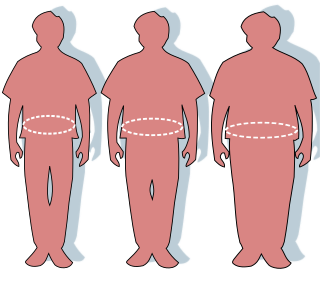
In addition to diet and exercise, weight loss is an important tool to help with diabetes management. T2D is often associated with obesity and increased abdominal circumference.[29] Often patients who are at risk of diabetes may be able to reverse their progression to T2D with weight loss as well.[29] Weight loss can help reduce the risk of further complications, other health related problems, and helps improve the effects of insulin on the body.[29][30] Weight loss helps reduce the destruction of the beta cells, which produce insulin in the body, as well.[29]
It is recommended for patients who have been diagnosed with T2D who are overweight or obese to lose at least 5% of their weight and maintain the weight loss. There have been studies that have demonstrated that by losing about 5 to 10% of their weight at diagnosis, there is a reduction in heart disease risk factors, lowered Hb A1c, less diabetes medications, lower cholesterol and improved fitness.[29] Additionally, patients who lose more weight are better off in the long run.[29]
Common strategies to help reduce weight many include lifestyle measures such as diet and exercise, behavioral therapy, pharmacologic interventions, and surgery. The goal of weight loss and method for achievement should be individualized based on the patient's desires and motivation.[29] It is important for providers to help maintain patient motivation to lose weight. Additionally, some medications that reduce blood sugars such as insulin may initially cause weight gain due to the increased conversion of blood sugar to stored forms such as fat.[29] Therefore, in patients with diabetes, providers may try other medications that lower blood sugar but not cause as much weight gain.[29]
Medications
Summarize
Perspective
There are several medications classes that are commonly used to control blood sugar levels in patients with diabetes. Most of the medications used are either oral or injected.[1] In patients with T1D, insulin is require because the body no longer produces insulin.[2] In patients with T2D, management is largely more variable as lifestyle changes can have a significant impact. However, medications may be added to further help control BG levels if the lifestyle changes are not effectively controlling the condition. Unlike type 1 diabetic patients, patients with T2D can still produce insulin, so usually these patients take oral medications first before requiring insulin for diabetic control.[2]
Patient education[31] and compliance with treatment is very important in managing the disease. Improper use of medications and insulin can be very dangerous causing hypo- or hyper-glycemic episodes.
Insulin

Insulin is the hormone that is made by the body that controls the cell intake of glucose. Normally, the pancreas produces insulin in response to high glucose levels in the body to bring the BG levels down. For type 1 diabetics, there will always be a need for insulin injections throughout their life, as the pancreatic beta cells of a type 1 diabetic are not capable of producing sufficient insulin.[32] Insulin can not be taken orally because insulin is a hormone and is destroyed by the digestive track. Insulin can be injected by several methods, including a hypodermic needle, jet injector, or insulin pump. There is also inhaled insulin that can be used in adults with diabetes.[33]
There are several types of insulin that are commonly used in medical practice, with varying times of onset and duration of action.[32]
- Rapid acting (i.e. insulin lispro) with onset in 15 minutes and duration of about 4 hrs.
- Short acting (i.e. regular insulin) with onset in 30 minutes and duration of about 6 hrs.
- Intermediate acting (i.e NPH insulin) with onset in 2 hours and duration of about 14 hrs.
- Long acting (i.e. detemir) with onset in 1 hr. and duration of about 24 hrs.
- Premixed which are usually combinations of short and long acting insulin.
Insulin is usually taken several times per day in patients who require it to control their diabetes.[32] Often patients usually take long acting insulin once a day and then take insulin before meals. The time of onset of the insulin determines how far in advance patients should take the insulin before they eat.[32]
Insulin therapy requires close monitoring and a great deal of patient education, as improper administration is quite dangerous. Insulin can easily cause hypoglycemia if the patient does not eat after administering insulin or accidentally had too much insulin.[32] A previously satisfactory dosing may be too much if less food is consumed causing hypoglycemia.[32] Exercise decreases insulin requirements as exercise increases glucose uptake by body cells whose glucose is controlled by the insulin.[21]
Insulin therapy creates risk because of the inability to continuously know a person's BG level and adjust insulin infusion appropriately. New advances in technology have overcome much of this problem. Small, portable insulin infusion pumps are available from several manufacturers. They allow a continuous infusion of small amounts of insulin to be delivered through the skin around the clock, plus the ability to give bolus doses when a person eats or has elevated BG levels. This is very similar to how the pancreas works, but these pumps lack a continuous "feed-back" mechanism. Thus, the user is still at risk of giving too much or too little insulin unless BG measurements are made.
Oral medications
Metformin
One of the most common drugs used in T2D, metformin is the drug of choice to help patients lower their blood sugar levels. Metformin is an example of a class of medicine called biguanides.[34] The medication works by reducing the new creation of glucose from the liver and by reducing absorption of sugar from food.[34] In addition, the medication also works to help increase the effects of insulin on muscle cells, which take in glucose.[35] The medicine is not used for T1D as these patients do not produce any insulin and metformin relies on some insulin production in order to be effective.[34] There are several preparations of the medication such as tablets, extend release tablets, and liquid suspensions. Metformin is usually started as 500 to 1000 mg tablets twice a day by mouth (PO), usually with meals.[34] If taking the extended release tablets, they should be always swallowed whole as cutting the tablet will cause faster release of the medication.[34] The medication most commonly may cause stomach upset and symptoms such as diarrhea but in general is well tolerated and has a relatively low chance of causing hypoglycemia.[35] One rare (about 1% chance) but serious side affect of metformin is that it can cause lactic acidosis, usually in patients with poor kidney function.[35] Sometimes, practitioners will slowly increase the dose of the medication to help with tolerance to the medication.
Sulfonylureas
Another commonly used class of medications with T2D are sulfonylureas. This class of medicine increases the release of insulin from the beta cells in the pancreas. The medication can not be used in patients with T1D, as they do not have functioning beta cells and can not produce insulin.[35] Some common example of a sulfonylurea is glipizide, glyburide, glimepiride and gliclazide. Depending on the medication, there are different size tablets but in general, the sizes range from about 1 mg to 10 mg. Usually the tablet is taken about 30 minutes before a meal and can be either once or twice a day. The most common adverse effects of the medication are lightheadedness and stomach irritation.[35] Sulfonylureas have a greater risk of hypoglycemia but the risk is still only around 3% of patients who use them.[35] In patients who have a greater risk of low sugar, such as in the elderly and patients with kidney disease, the starting dose can be as low as 0.5 mg.
GLP-1 agonists
Another popular medication that is used in T2D management are glucagon like peptide 1 (GLP-1) agonists. This class of medication works by mimicking a hormone called glucagon-like peptide which has many effects in the body.[36] One effect of the hormone is that it helps time the release of insulin when patients eat and the BG rises.[37] In addition, it can significantly increase the amount of insulin release as well.[38] Lastly, the medication also slows down the movement of food through the digestive tract and can increase feeling of fullness while eating, decreasing appetite and weight.[37] These drugs are very effective at controlling T2D and reducing risk of heart attacks, strokes, and other complications due to diabetes. In addition, patients usually lose weight and have improved blood pressure and cholesterol.[36] Common names of these medications include semaglutide (Ozempic and Wegovy), liraglutide (Victoza, Saxenda), and dulaglutide (Trulicity).[36] These medications must be injected and are usually injected in the upper arm, thighs or stomach areas.[37] They are usually given once a week but some of the medication can be as frequent as twice daily.[36] The dose is usually started low and tapered gradually. Some of the common side effects of the medication is nausea, vomiting and diarrhea. Patients with a family history of medullary thyroid cancer or Multiple Endocrine Neoplasia type 2 should not be prescribed the drug may increase the risk of developing cancer.[37]
Surgery
Summarize
Perspective
While weight loss is clearly beneficial in improving glycemic control in patients with diabetes type 2,[39] maintaining significant weight loss can be a very difficult thing to do. In diabetic people who have a body mass index of 35 or higher, and who have been unable to lose weight otherwise, bariatric surgery offers a viable option to help achieve that goal. In 2018 a Patient-Centered Outcomes Research Institute funded study was published which analyzed the effects of three common types of bariatric surgery on sustained weight loss and long-lasting glycemic control in patients with diabetes type 2.[40] The results of this study demonstrated that, five years after bariatric surgery, there was meaningfully significant weight loss in a large majority of patients. In addition, and more importantly, this study showed that, in type 2 diabetic patients with a body mass index of 35 or higher, bariatric surgery has the potential to lead to complete remission of diabetes in as many as 40% of those people who have the procedure.[41] Like any operation, bariatric surgery is not without risks and complications, and those risks need to weighed against the potential benefits in anyone considering going through with such a procedure.
Additional monitoring
Summarize
Perspective
Foot checking
Monitoring a person's feet can help in predicting the likelihood of developing diabetic foot ulcers. A common method for this is using a special thermometer to look for spots on the foot that have higher temperature which indicate the possibility of an ulcer developing.[42] At the same time there is no strong scientific evidence supporting the effectiveness of at-home foot temperature monitoring.[43]
The current guideline in the United Kingdom recommends collecting 8-10 pieces of information for predicting the development of foot ulcers.[44] A simpler method proposed by researchers provides a more detailed risk score based on three pieces of information (insensitivity, foot pulse, previous history of ulcers or amputation). This method is not meant to replace people regularly checking their own feet but complement it.[42][45]
Dental care
High BG in diabetic people is a risk factor for developing gum and tooth problems. Diabetic patients have greater chances of developing oral health problems such as tooth decay, saliva production dysfunction, fungal infections, and periodontal disease[46] Diabetic people tend to experience more severe periodontitis because diabetes lowers the ability to resist infection and also slows healing.[47] In turn, the chronic infection from periodontal disease can make it worse to control the diabetes, leading to worsening of diabetic complications.[48] The oral problems in persons with diabetes can be prevented with a good control of the blood sugar levels, regular check-ups with their dental provider, and good oral hygiene. Looking for early signs of gum disease (redness, swelling, bleeding gums) and informing the dentist about them is also helpful in preventing further complications. Quitting smoking is recommended to avoid serious diabetes complications and oral diseases. By maintaining a good oral status, diabetic persons prevent losing their teeth as a result of various periodontal conditions.
Digital tools
Electronic health records
Sharing their electronic health records with people who have T2D helps them to reduce their blood sugar levels. It is a way of helping people understand their own health condition and involving them actively in its management.[49][50]
m-health monitoring applications
The widespread use of smartphones has turned mobile applications (apps) into a popular means of the usage of all forms of software.[51] The number of health-related apps accessible in the App Store and Google Play is approximately 100,000, and among these apps, the ones related to diabetes are the highest in number. Conducting regular self-management tasks such as medication and insulin intake, blood sugar checkup, diet observance, and physical exercise are really demanding.[52] This is why the use of diabetes-related apps for the purposes of recording diet and medication intake or BG level is promising to improve the health condition for the patients.
Complexities
Summarize
Perspective

The main complexities stem from the nature of the feedback loop of glucose in the blood stream.
- The glucose cycle is a system which is affected by two factors: entry of glucose into the bloodstream and also blood levels of insulin to control its transport out of the bloodstream
- As a system, it is sensitive to diet and exercise
- It is affected by the need for patient anticipation due to the complicating effects of time delays between any activity and the respective impact on the glucose
- Management is highly intrusive, and compliance is an issue, since it relies upon user lifestyle change and often upon regular sampling and measuring of BG levels, multiple times a day in many cases
- It changes as people grow and develop
- It is highly individual
As diabetes is a prime risk factor for cardiovascular disease, controlling other risk factors which may give rise to secondary conditions, as well as the diabetes itself, is one of the facets of diabetes management. Checking cholesterol, LDL, HDL and triglyceride levels may indicate hyperlipoproteinemia, which may warrant treatment with hypolipidemic drugs. Checking the blood pressure and keeping it within strict limits (using diet and antihypertensive treatment) protects against the retinal, renal and cardiovascular complications of diabetes. Regular follow-up by a podiatrist or other foot health specialists is encouraged to prevent the development of diabetic foot. Annual eye exams are suggested to monitor for progression of diabetic retinopathy.[53]
Hypoglycemia

A level of <70 mg/dL (<3.8 mmol/L) is described as a hypoglycemic attack (low blood sugar). Most diabetics know when they are hypoglycemic and seek food or a sweet drink to raise their glucose levels. Intensive efforts to achieve blood sugar levels close to normal have been shown to triple the risk of the most severe form of hypoglycemia, in which the person requires assistance from by-standers in order to treat the episode.[54] Among intensively controlled type 1 diabetics, 55% of episodes of severe hypoglycemia occur during sleep, and 6% of all deaths in diabetics under the age of 40 are from hypoglycemia at night.[55]
Hypoglycemia can be problematic if it occurs while driving as it can affect a person's thinking process, coordination, and state of consciousness.[56][57] Some people are more prone to hypoglycemia as they have reported fewer warning symptoms, and their body released less epinephrine (a hormone that helps raise blood glucose).[58] Additionally, individuals with a history of hypoglycemia-related driving mishaps appear to use sugar at a faster rate.[59]
Drivers with diabetes susceptible to driving mishaps should monitor their blood sugar to be not less than 70 mg/dL (3.9 mmol/L). Instead, these drivers are advised to treat hypoglycemia and delay driving until their blood glucose is above 90 mg/dL (5 mmol/L).[58]
Hyperglycemia
A patient is considered to have hyperglycemia (high glucose) if the patient has a sugar level of greater than 230–270 mg/dL (13–15 mmol/L). Sometimes patient may be temporarily hypoglycemic under certain conditions (e.g. not eating regularly, or after strenuous exercise). Patients should closely monitor their sugar levels to ensure that they reduce rather than continue to remain high. High blood sugar levels are not as easy to detect as hypoglycemia and usually happens over a period of days rather than hours or minutes. If left untreated, this can result in diabetic coma and death.
Prolonged and elevated levels of glucose in the blood, which is left unchecked and untreated, will, over time, result in serious diabetic complications in those susceptible and sometimes even death. There is currently no way of testing for susceptibility to complications. Diabetics are therefore recommended to check their blood sugar levels either daily or every few days. There is also diabetes management software available from blood testing manufacturers which can display results and trends over time.
Medication nonadherence
Because many patients with diabetes have two or more comorbidities, they often require multiple medications. The prevalence of medication nonadherence is high among patients with chronic conditions, such as diabetes, and nonadherence is associated with public health issues and higher health care costs. One reason for nonadherence is the cost of medications. Being able to detect cost-related nonadherence is important for health care professionals, because this can lead to strategies to assist patients with problems paying for their medications. Some of these strategies are use of generic drugs or therapeutic alternatives, substituting a prescription drug with an over-the-counter medication, and pill-splitting. Interventions to improve adherence can achieve reductions in diabetes morbidity and mortality, as well as significant cost savings to the health care system.[60] Smartphone apps have been found to improve self-management and health outcomes in people with diabetes through functions such as specific reminder alarms,[61] while working with mental health professionals has also been found to help people with diabetes develop the skills to manage their medications and challenges of self-management effectively.[62]
Psychological mechanisms and adherence
As self-management of diabetes typically involves lifestyle modifications, adherence may pose a significant self-management burden on many individuals.[63] For example, individuals with diabetes may find themselves faced with the need to self-monitor their BG levels, adhere to healthier diets and maintain exercise regimens regularly in order to maintain metabolic control and reduce the risk of developing cardiovascular problems. Barriers to adherence have been associated with key psychological mechanisms: knowledge of self-management, beliefs about the efficacy of treatment and self-efficacy/perceived control.[63] Such mechanisms are inter-related, as one's thoughts (e.g. one's perception of diabetes, or one's appraisal of how helpful self-management is) is likely to relate to one's emotions (e.g. motivation to change), which in turn, affects one's self-efficacy (one's confidence in their ability to engage in a behaviour to achieve a desired outcome).[64]
As diabetes management is affected by an individual's emotional and cognitive state, there has been evidence suggesting the self-management of diabetes is negatively affected by diabetes-related distress and depression.[65] There is growing evidence that there is higher levels of clinical depression in patients with diabetes compared to the non-diabetic population.[66][67] Depression in individuals with diabetes has been found to be associated with poorer self-management of symptoms.[68] This suggests that it may be important to target mood in treatment. In the case of children and young people, especially if they are socially disadvantaged, research suggests that it is important that healthcare providers listen to and discuss their feelings and life situation to help them engage with diabetes services and self-management.[69][70]
To this end, treatment programs such as the Cognitive Behavioural Therapy - Adherence and Depression program (CBT-AD)[62] have been developed to target the psychological mechanisms underpinning adherence. By working on increasing motivation and challenging maladaptive illness perceptions, programs such as CBT-AD aim to enhance self-efficacy and improve diabetes-related distress and one's overall quality of life.[71]
See also
References
External links
Wikiwand - on
Seamless Wikipedia browsing. On steroids.